What Are Drug Interactions and Why They Matter for Medication Safety
 Jan, 15 2026
Jan, 15 2026
Every year, thousands of people end up in hospitals not because their condition got worse, but because something they took to feel better made something else they were taking dangerous. This isn’t rare. It’s called a drug interaction, and it’s one of the most preventable causes of harm in modern medicine.
What Exactly Is a Drug Interaction?
A drug interaction happens when one substance changes how another substance works in your body. That substance could be another prescription drug, an over-the-counter medicine, a vitamin, a herbal supplement, even your morning grapefruit juice. It doesn’t mean the drugs are bad. It means they don’t always play nice together. There are three main types:- Drug-drug interactions: When two or more medications affect each other. For example, taking the blood thinner warfarin with certain antibiotics can make your blood too thin, leading to dangerous bleeding.
- Drug-food/drink interactions: Certain foods or drinks can change how your body absorbs or breaks down a drug. Grapefruit juice is the most famous offender-it can cause statins like simvastatin to build up to toxic levels, leading to muscle damage or kidney failure.
- Drug-condition interactions: Your existing health problems can make a drug riskier. For instance, taking NSAIDs like ibuprofen if you have kidney disease can worsen kidney function.
These aren’t just theoretical risks. In the U.S., drug interactions contribute to over 1.3 million emergency room visits and 350,000 hospital admissions every year. That’s more than many common infections.
Why Do These Interactions Happen?
Your body has a system for processing drugs-mainly through the liver and kidneys. The liver uses enzymes, especially the CYP450 family, to break down medications so your body can get rid of them. One enzyme, CYP3A4, handles about half of all prescription drugs. When another drug or substance blocks or speeds up this enzyme, it throws off the balance. For example:- Fluconazole (an antifungal) blocks CYP3A4. If you take it with simvastatin (a cholesterol drug), your simvastatin levels can spike by up to 2,000%. That’s not a small change-it’s a medical emergency waiting to happen.
- Some antibiotics like clarithromycin do the same thing. That’s why doctors avoid prescribing them together.
Then there’s the second kind: pharmacodynamic interactions. This is when two drugs hit the same target in your body and either:
- Add up (like taking two sleeping pills and passing out)
- Cancel each other out (like NSAIDs making diuretics less effective by causing fluid retention)
- Work against each other (like beta-blockers making asthma inhalers less effective)
Some interactions are so dangerous they’re labeled “contraindicated”-meaning you should never mix them. Others are “significant,” requiring close monitoring. And some are minor, like a slight delay in absorption.
Which Medications Are Most Likely to Cause Problems?
Not all drugs are equal when it comes to interactions. Some are like minefields. The top three are:- Warfarin (Coumadin): This blood thinner has over 600 known interactions. Even something as simple as cranberry juice or a new antibiotic can make your INR (a blood test that measures clotting) swing dangerously. One wrong combination can lead to internal bleeding-or, if the interaction makes warfarin less effective, a stroke.
- Digoxin (Lanoxin): Used for heart rhythm problems, digoxin interacts with antibiotics, diuretics, and even some heart medications. A tiny change in blood levels can cause nausea, confusion, or life-threatening arrhythmias.
- Levothyroxine (Synthroid): This thyroid hormone is absorbed poorly if taken with calcium, iron, or even coffee. Many people take it with breakfast, unaware that their multivitamin is blocking its effect-leaving them tired, gaining weight, and feeling off.
These aren’t obscure drugs. Millions take them daily. And most patients have no idea how many things can interfere with them.
How Common Are These Problems?
The numbers are startling. In the U.S., drug interactions cause about 6.5% of all hospital admissions. For people over 65, the risk is three times higher. Why? Because older adults take an average of 4.7 prescription drugs a day. Add in supplements, OTC painkillers, and herbal remedies, and you’ve got a cocktail no one fully checked.A 2022 study in JAMA Internal Medicine found that serious drug interactions lead to around 106,000 deaths annually in the U.S. alone. That’s more than traffic accidents. And it’s mostly preventable.
Even more alarming: only 25% of dangerous interactions are found during clinical trials. Why? Because trials exclude older people, those with multiple conditions, and people taking many medications. So when the drug hits the real world, the risks emerge-and people get hurt.

What About Food and Supplements?
Grapefruit juice isn’t the only food that causes trouble. Here are a few others:- Leafy greens (kale, spinach, broccoli) are high in vitamin K, which directly opposes warfarin’s effect. Sudden changes in intake can make your blood clot too easily or not enough.
- Dairy products and calcium supplements can block absorption of antibiotics like tetracycline and fluoroquinolones, making them useless.
- Alcohol can increase drowsiness with sedatives, raise blood pressure with antidepressants, and damage the liver when mixed with acetaminophen.
- St. John’s Wort, a popular herbal remedy for mild depression, speeds up the breakdown of dozens of drugs-including birth control pills, antidepressants, and even some cancer treatments-making them ineffective.
And supplements? They’re not regulated like drugs. A “natural” product can still be dangerous. Many people assume if it’s sold in a health food store, it’s safe. That’s a dangerous myth.
Who’s at the Highest Risk?
You might think this only affects older people. But anyone taking multiple medications is at risk. High-risk groups include:- People over 65: 45% of serious drug interaction events happen in this group, even though they make up only 16% of the population.
- Those with five or more chronic conditions: 68% of them experience at least one significant interaction.
- Patients on drugs metabolized by CYP3A4, CYP2D6, or CYP2C9 enzymes: These handle 70% of all prescription medications.
- People seeing multiple doctors: If your cardiologist, rheumatologist, and GP aren’t talking, your meds might be a minefield.
One patient in Brighton told me she was prescribed a new antibiotic for a sinus infection. She didn’t tell her pharmacist she was also taking a blood pressure pill and a cholesterol drug. Within days, she had severe muscle pain and was hospitalized. Her doctor later found the antibiotic had raised her statin levels to dangerous levels.
How Can You Protect Yourself?
You don’t need to be a doctor to avoid these risks. Here’s what works:- Keep a full list of everything you take: Prescription drugs, OTC meds, vitamins, herbs, even cough syrups. Include dosages and how often you take them.
- Use one pharmacy: Pharmacists have tools that check for interactions across all your meds. If you switch pharmacies, you lose that safety net.
- Ask your pharmacist every time: Don’t assume your doctor knows about every supplement you take. Pharmacists are trained to catch interactions. They catch about 3.5 million drug-related problems every year in the U.S.-22% of them are interactions.
- Check for interactions yourself: Use free, reliable tools like the FDA-approved GoodRx Drug Interaction Checker or Medscape’s tool (used by 78% of U.S. physicians). Don’t rely on random websites.
- Take meds at the right time: Some drugs need to be taken 2 hours before or after food or supplements. Levothyroxine? Take it on an empty stomach, at least 30-60 minutes before eating.
- Don’t stop or start anything without asking: Even “harmless” things like magnesium or fish oil can interfere.
What’s Being Done to Fix This?
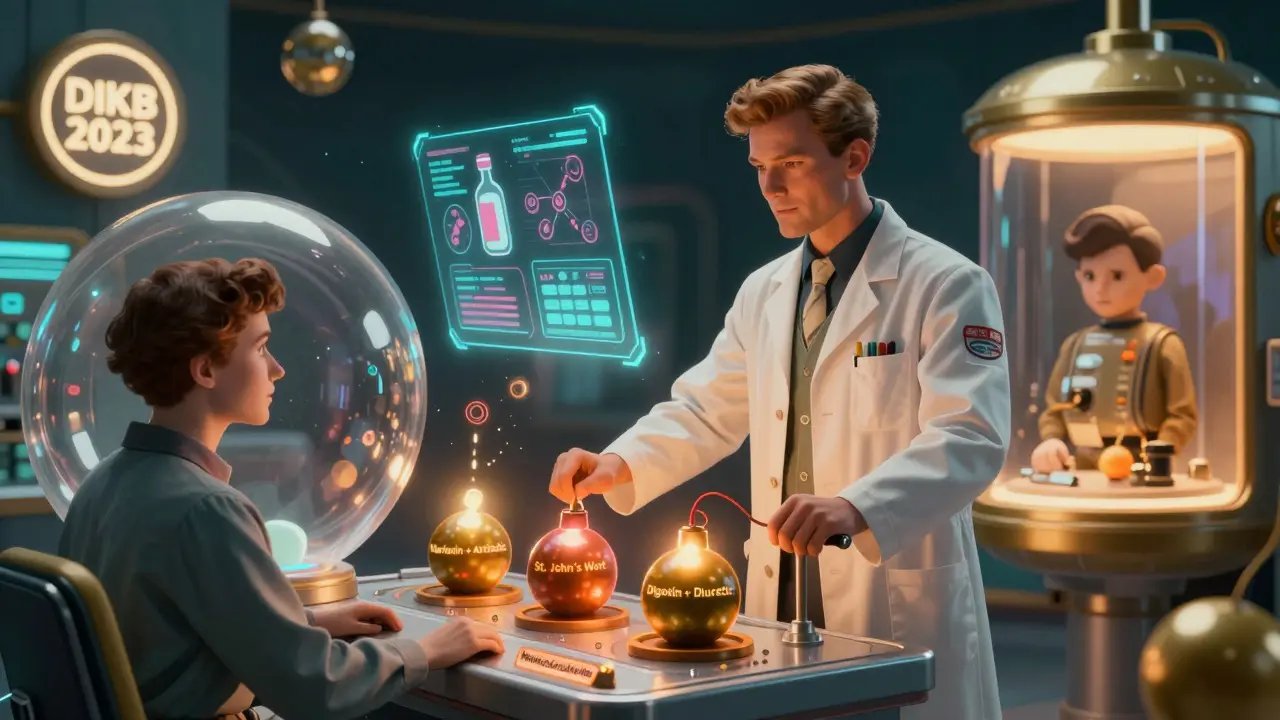
Hospitals and pharmacies are slowly improving. Most U.S. hospitals now use electronic records with basic interaction alerts. But only 42% have systems that give real-time, severity-ranked warnings. That means many alerts are ignored because they’re too vague.The FDA launched the Drug Interaction Knowledgebase (DIKB) in 2023-a machine-readable database with 12,000+ verified interactions and evidence levels. That’s a big step forward.
And the future? Personalized medicine. Genetic testing for CYP450 enzymes is already being used for some drugs. By 2026, it’s expected to become standard for high-risk medications. Imagine knowing your body breaks down drugs slowly-and getting a lower dose before you even start.
But until then, the burden falls on you.
Final Thought: This Isn’t About Fear-It’s About Control
Drug interactions aren’t a reason to avoid medicine. They’re a reason to be smarter about it. Medications save lives. But they can also harm you if you don’t understand how they work together.Take charge. Keep your list. Talk to your pharmacist. Ask questions. Don’t let a simple interaction turn into a hospital stay-or worse.
Can over-the-counter medications cause drug interactions?
Yes. Common OTC drugs like ibuprofen, naproxen, antacids, and even cold medicines can interact with prescription drugs. For example, taking ibuprofen with blood pressure medication can reduce its effectiveness. Taking antacids with antibiotics like ciprofloxacin can stop the antibiotic from being absorbed. Always check OTC meds the same way you check prescriptions.
Are herbal supplements safe to take with prescription drugs?
Not necessarily. Many herbal supplements interfere with how drugs work. St. John’s Wort can make birth control, antidepressants, and transplant drugs fail. Garlic and ginkgo can increase bleeding risk with blood thinners. Green tea can affect how some cancer drugs are processed. Just because something is “natural” doesn’t mean it’s safe with your meds.
Why does grapefruit juice affect some drugs but not others?
Grapefruit contains compounds called furanocoumarins that block an enzyme in the gut called CYP3A4. This enzyme breaks down certain drugs before they enter the bloodstream. If it’s blocked, the drug builds up to dangerous levels. But not all drugs rely on this enzyme. Statins like simvastatin and atorvastatin are affected, but rosuvastatin isn’t. Always check whether your specific drug is on the list.
Can drug interactions happen even if I take my meds at different times of day?
Yes. Some interactions aren’t about timing-they’re about how your body processes the drug long-term. For example, if you take an antibiotic that blocks liver enzymes, it can raise levels of another drug for days after you stop the antibiotic. That’s why it’s not enough to just space them out. You need to know if the interaction is pharmacokinetic (body processing) or pharmacodynamic (effect on the body).
How do I know if a drug interaction is serious enough to worry about?
Look for labels like “contraindicated,” “major,” or “severe” in interaction checkers. Symptoms like unusual bruising, muscle pain, dizziness, confusion, or rapid heartbeat can signal a problem. If you’re unsure, call your pharmacist. They can tell you if it’s something to monitor or something that requires an immediate change.
What to Do Next
Start today. Grab a piece of paper or open a note on your phone. Write down every medication, supplement, and vitamin you take-name, dose, and time of day. Take it to your next doctor or pharmacy visit. Ask: “Could any of these interact?”Don’t wait for a hospital visit to learn the hard way. Medication safety isn’t about trusting your doctor alone. It’s about knowing your own body-and asking the right questions.

brooke wright
January 16, 2026 AT 20:26My grandma took warfarin and started drinking cranberry juice because she heard it was 'heart-healthy.' One morning she passed out on the bathroom floor. Turned out her INR was through the roof. She spent a week in the hospital. No one told her juice could kill you. Now she keeps a list. So should you.
And yes, I'm still mad at the pharmacist who didn't ask about her smoothies.
evelyn wellding
January 18, 2026 AT 14:09YESSSS this is so important!! 🙌 I used to take St. John’s Wort with my antidepressant because 'it’s natural!' Then I felt like a zombie and my anxiety went nuclear. My pharmacist caught it during a refill. I was so embarrassed… but now I check EVERYTHING. Even that gummy vitamin I take. 💊❤️
Chelsea Harton
January 19, 2026 AT 02:47grapefruit is a traitor. and so is coffee. and so am i for taking tylenol with wine. 🤦♀️
Corey Chrisinger
January 19, 2026 AT 03:18It’s wild how we treat our bodies like machines that can handle any input, but we’d never throw random parts into a Ferrari and expect it to run. We’re biological systems with intricate enzyme pathways, and yet we think popping a supplement is like adding sugar to coffee.
Maybe the real problem isn’t the drugs-it’s the assumption that we’re in control when we’re not.
Also, 🤔 what if our entire medical system is built on ignoring complexity?
Bianca Leonhardt
January 19, 2026 AT 21:04Of course you’re surprised people are getting hospitalized. You think your 'natural remedies' are safe? You’re not special. You’re just statistically likely to die from something dumb. If you can’t read a label, don’t take the pill. Simple.
And yes, I’m talking to you, the person who takes fish oil, turmeric, and melatonin with your blood pressure med. You’re one ER visit away from becoming a case study.
Travis Craw
January 21, 2026 AT 01:18I didn’t know grapefruit messed with statins until my mom had to go to the ER. She’s 72, takes 7 meds, and swears she doesn’t need to tell her doctor about her 'little vitamins.'
Now I print out interaction charts for her every time she gets a new script. She rolls her eyes but she keeps them on the fridge. Small wins, right?
Also, one pharmacy rule: ALWAYS use the same one. It’s the only thing that’s kept me alive so far.
Christina Bilotti
January 21, 2026 AT 21:40Oh sweetie, you think you’re the first person to discover that 'natural' doesn’t mean 'safe'? Let me guess-you also think probiotics cure cancer and that magnesium is a miracle. Honey, your supplements are just expensive glitter.
And yes, I’ve seen your Instagram stories. The one where you’re holding up a bottle of 'immune-boosting mushroom powder' with your coffee and ibuprofen. You’re not a wellness influencer. You’re a walking adverse event waiting to happen.
Cheryl Griffith
January 22, 2026 AT 03:22This hit me hard. My dad had a stroke last year because his blood thinner interacted with an OTC cold med he thought was 'fine.' He didn’t tell anyone because he didn’t want to 'bother' the doctor.
Now I make him read his meds list out loud to me every Sunday. He hates it. But he’s alive.
If you’re reading this and you’re scared to ask your pharmacist a question-just do it. They’ve seen it all. They won’t judge you. They’ll just save your life.
Nick Cole
January 22, 2026 AT 17:52One time I took ibuprofen with my blood pressure med because my back hurt. Didn’t think twice. Two days later I was dizzy and my kidneys were acting up.
My doctor said, 'You’re lucky you didn’t crash.'
Now I have a sticky note on my pill organizer that says: 'ASK BEFORE YOU SWALLOW.'
It’s not paranoia. It’s survival.
Bobbi-Marie Nova
January 23, 2026 AT 07:35Okay but can we talk about how ridiculous it is that we have to be pharmacists just to not die? 🤦♀️ I mean, I get it-pharma’s complicated. But shouldn’t the system be designed to protect us instead of making us google our meds like detectives?
Also, I now keep a Google Doc titled 'My Meds Are Not a Game' and I update it after every doctor visit. It’s my little rebellion against chaos. 💪
Allen Davidson
January 24, 2026 AT 00:07This post saved my life. Not hyperbole. I was on 8 meds, took St. John’s Wort for 'mild anxiety,' and didn’t realize it was making my antidepressant useless. My mood tanked. I thought I was failing. Turns out, my liver was just busy breaking it down.
I went to my pharmacist, showed her my list, and she said, 'You’re not crazy-you’re just overdosed on misinformation.'
Now I bring my list to every appointment. No excuses. If you’re on more than 3 meds, do this. Your future self will thank you.
And yes, I still drink grapefruit juice. But only after checking the label. 🍊✅