Warfarin Side Effects and Bleeding Risks: What You Must Know as a Patient
 Dec, 30 2025
Dec, 30 2025
Warfarin Bleeding Risk Calculator
Assess Your Bleeding Risk
Enter your current details to calculate your risk level for major bleeding while taking warfarin.
Warfarin has been used for over 70 years to prevent dangerous blood clots. It’s one of the most common blood thinners prescribed in the UK and the US, especially for people with atrial fibrillation, deep vein clots, or mechanical heart valves. But while it works, it’s not without serious risks. Warfarin side effects can be life-threatening - especially bleeding. If you’re taking warfarin, you need to know what to watch for, when to act, and how to stay safe every single day.
What Warfarin Does - and Why It’s Still Used
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Without those factors, blood doesn’t clot as easily. That’s good if you’re at risk of stroke or a pulmonary embolism. But it’s dangerous if you cut yourself, fall, or develop an internal bleed.
Despite newer blood thinners like apixaban and rivaroxaban, warfarin is still widely used. Why? It’s cheap - generic warfarin costs about £3 to £8 a month in the UK. It’s also reversible. If you start bleeding badly, doctors can give you vitamin K or a concentrated clotting factor to reverse its effects quickly. Newer drugs don’t have that advantage. For some people - like those with mechanical heart valves - warfarin is still the only safe option.
The Biggest Risk: Bleeding
Bleeding is the #1 danger with warfarin. About 1 in 10 people on warfarin will have a major bleed each year. That’s not rare. It’s common enough that every patient needs to treat it like a medical emergency.
Minor bleeding might seem harmless - a nosebleed that lasts longer than 5 minutes, bleeding gums when brushing your teeth, or unexplained bruises. But these are warning signs. They mean your blood is taking too long to clot.
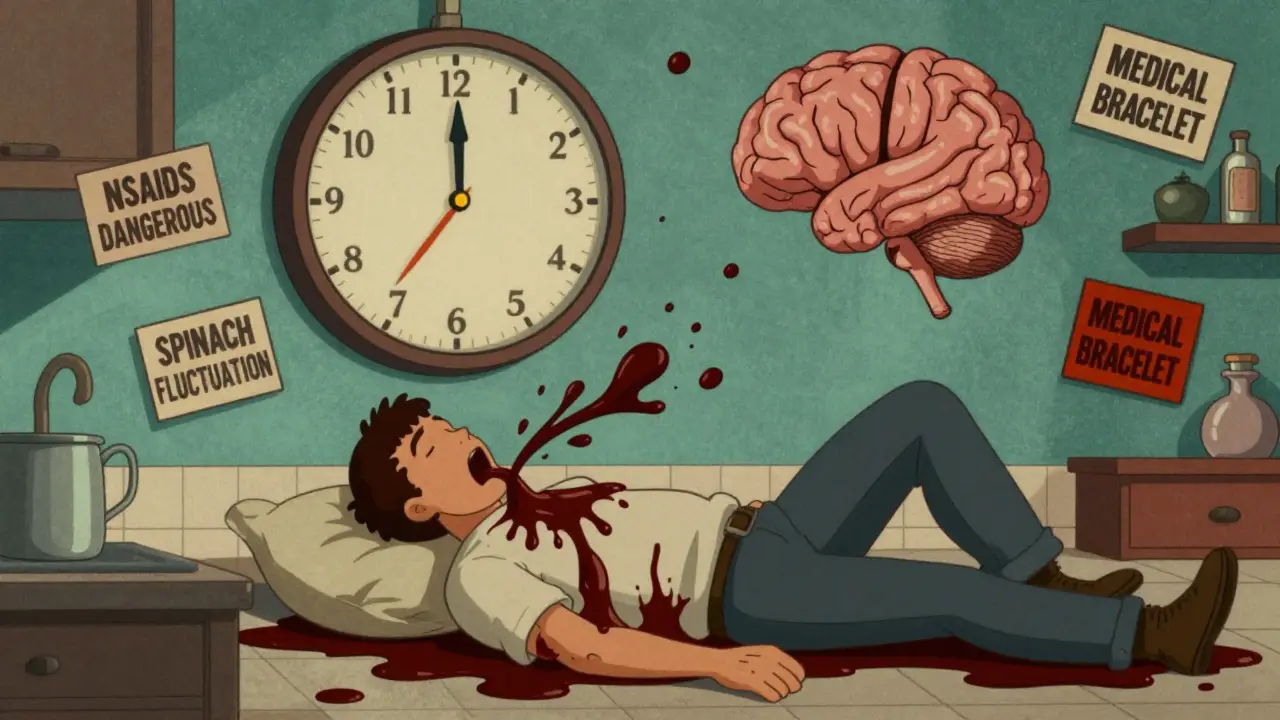
Major bleeding is far more serious. Call 999 or go to A&E if you have:
- Red, pink, or brown urine
- Black, tarry, or bloody stools
- Vomiting blood or material that looks like coffee grounds
- Sudden, severe headache or dizziness
- Weakness on one side of your body
- Severe back or abdominal pain
- Heavy vaginal bleeding outside your period
- Any bleeding that won’t stop after 10 minutes of pressure
These symptoms can mean internal bleeding - in your brain, gut, or around your organs. Brain bleeds are especially deadly. About 0.2% to 0.5% of warfarin users have one each year. The faster you get help, the better your chances.
Your INR Is Your Lifeline
Doctors measure how well warfarin is working with a blood test called INR (International Normalized Ratio). The goal is usually between 2.0 and 3.0. For people with mechanical heart valves, it might be higher - around 2.5 to 3.5.
Here’s the key: every point your INR goes above 3.0 doubles your risk of major bleeding. At INR 4.0, your risk is 4 to 8 times higher than when you’re in range. That’s why regular testing matters.
If your INR is stable, you’ll usually get tested every 4 weeks. But if you’ve just started warfarin, changed your dose, or been sick, you might need testing every week. Some people even test at home with a finger-prick device like the CoaguChek Pro II. Studies show this can improve your time in range by 15% to 20% - meaning fewer bleeds and fewer hospital visits.
What Makes Bleeding Worse
Some risks you can’t change. Age over 65? That doubles your bleeding risk. History of stomach ulcers? That triples it. High blood pressure? That increases risk by almost 3 times. If you have three or more of these risk factors, your chance of a major bleed jumps to nearly 20% per year.
But some risks you can control:
- INR too high - the biggest modifiable risk. Never skip your blood tests.
- Medications - NSAIDs like ibuprofen and naproxen can increase stomach bleeding risk by 2 to 4 times when taken with warfarin. Use paracetamol instead, unless your doctor says otherwise.
- Diet changes - eating a big bowl of spinach or kale one day and none the next can swing your INR by 0.5 to 1.0 points. Keep your vitamin K intake steady. Aim for 60-80 mcg daily. That means consistent portions of leafy greens - not none, not tons.
- Alcohol - heavy drinking can make your INR go up and down unpredictably. Stick to moderate amounts, if any.
- Supplements - garlic, ginkgo, fish oil, and even some herbal teas can thin your blood further. Always tell your doctor what you’re taking.
Rare but Serious Side Effects
Bleeding isn’t the only problem. Warfarin can cause rare but scary side effects.
Warfarin-induced skin necrosis - This happens in about 1 in 10,000 people. Within days of starting warfarin, you might see dark, painful patches of skin, usually on the thighs, breasts, or buttocks. It’s linked to a sudden drop in protein C, a natural anticoagulant. If you see this, stop the drug and get to a hospital immediately.
Purple toe syndrome - A few weeks after starting warfarin, your toes might turn purple or blue. It’s caused by tiny cholesterol crystals blocking blood vessels. It’s not life-threatening, but it’s painful and needs medical attention.
Calciphylaxis - This is extremely rare, mostly in people with kidney failure. Calcium builds up in small blood vessels, causing painful skin ulcers. If you have kidney disease and notice hard, painful spots on your legs, tell your doctor right away.
How to Stay Safe Every Day
Living on warfarin isn’t about fear - it’s about smart habits.
- Use an electric razor, not a blade. Blades cause small cuts you won’t notice - but they can bleed longer.
- Use a soft-bristle toothbrush and waxed floss. Don’t brush hard. Gum bleeding is common - but if it doesn’t stop, call your doctor.
- Avoid contact sports. No rugby, football, boxing, or skiing without proper protection. Even biking carries fall risk.
- Wear a medical alert bracelet or carry a card that says you’re on warfarin. In an emergency, that saves lives.
- Always tell any doctor, dentist, or pharmacist you’re on warfarin - even for a simple filling. Some procedures need temporary adjustments.
- Keep a log of your INR results, doses, and any symptoms. It helps your doctor spot patterns.

What to Do If You Bleed
Minor bleeding - like a small nosebleed that stops in under 5 minutes - usually doesn’t need emergency care. But call your anticoagulation clinic. They might want to check your INR.
For serious bleeding, don’t wait. Call 999. Don’t try to drive yourself. Emergency teams will:
- Test your INR right away
- Stop your warfarin
- Give you vitamin K (by injection) to reverse the effect
- Use prothrombin complex concentrate (PCC) if bleeding is life-threatening - this works in minutes
If you have a brain bleed, reversal must happen within 30 to 60 minutes. Every minute counts.
When to Consider Switching
Newer blood thinners - called DOACs - are now first-choice for most people with atrial fibrillation or clots. They don’t need regular INR checks, have fewer food interactions, and carry about 30% less risk of major bleeding than warfarin.
But they’re not for everyone. If you have a mechanical heart valve, severe kidney disease, or are pregnant, warfarin is still the best option. Your doctor should review your situation every year. Ask: “Is warfarin still the right choice for me?”
Bottom Line: Stay Informed, Stay Vigilant
Warfarin saves lives - but it can also end them if not managed carefully. The good news? You’re not helpless. You have control. Test your INR. Eat consistently. Avoid risky meds. Watch for bleeding. Speak up.
Most people on warfarin live full, active lives - as long as they stay informed and follow their plan. Don’t ignore the small signs. Don’t skip the tests. Don’t assume it’s fine because you feel okay. Bleeding doesn’t always come with pain. Sometimes, it just comes with a bruise, a nosebleed, or a change in your urine.
Know the signs. Know your numbers. And never, ever stop taking warfarin without talking to your doctor first.

John Chapman
December 30, 2025 AT 22:27Just started warfarin last month after my AFib diagnosis. 🤯 I was terrified at first, but this post literally saved my life. I didn’t know about the INR doubling risk above 3.0 - now I check my app every week. Also, switched to paracetamol instead of ibuprofen. No more headaches about meds. 🙌
Urvi Patel
December 31, 2025 AT 14:42Wow so much handholding here. People on warfarin need to be adults not toddlers. If you can’t manage a blood thinner you shouldn’t be on one. Also vitamin K isn’t rocket science eat spinach every day or don’t. Done.
Harriet Hollingsworth
December 31, 2025 AT 16:32I’m sorry, but this article is dangerously misleading. It implies that warfarin is somehow ‘safe’ if you ‘follow the rules.’ That’s not true. Bleeding risks are inherent. And the suggestion that home INR testing improves outcomes? That’s a pharma-funded myth. I’ve seen patients die because they trusted their ‘convenient’ device over a real lab. Don’t be fooled.
Bennett Ryynanen
January 1, 2026 AT 05:19Bro I was on warfarin for 3 years after my pulmonary embolism. I lost 20 pounds because I couldn’t eat anything without checking the vitamin K content. My wife made me a spreadsheet. We even had a ‘K-day’ every Sunday. But here’s the thing - I’m alive. And I can still hike, play with my kids, and laugh. It’s not easy, but it’s worth it. You got this.
Chandreson Chandreas
January 1, 2026 AT 17:27Life is just a series of trade-offs, right? Warfarin gives you time - but steals your freedom to eat salad without fear. Maybe the real question isn’t ‘how to survive warfarin’ but ‘why do we still rely on a 70-year-old drug when nature gave us better tools?’ 🤔
Darren Pearson
January 2, 2026 AT 05:24While the information presented is generally accurate, it lacks sufficient citation of peer-reviewed literature. For instance, the claim that home INR monitoring improves time in therapeutic range by 15–20% is derived from a 2017 meta-analysis in the Journal of Thrombosis and Haemostasis - a study with notable selection bias. Without proper context, such statistics may mislead patients.
Stewart Smith
January 2, 2026 AT 13:57So you’re telling me I have to eat the same amount of kale every day… or risk bleeding out? Cool. I’ll just stick to pizza. 🍕
Retha Dungga
January 2, 2026 AT 20:13Warfarin is just another way the system keeps us docile. They give us poison then tell us to measure it like good little robots. But what if we just… didn’t take it? What if the body knows better than the lab?
Jenny Salmingo
January 3, 2026 AT 16:11I’m from a small town in Texas. My grandma took warfarin for 12 years. She never missed a test. She ate spinach every Tuesday. She wore her bracelet even to church. She’s 89 and still dances at weddings. If she can do it, so can you. 💪
Aaron Bales
January 4, 2026 AT 14:38Stop skipping INR tests. That’s the #1 mistake. Period.
Lawver Stanton
January 5, 2026 AT 15:22Okay so I’ve been on warfarin for 5 years and I’m just now realizing that I’ve been eating kale like it’s going out of style. I mean, I had a smoothie with 3 cups of spinach every morning. And I thought I was being healthy. Turns out I was basically fighting my own blood thinner. My INR was all over the place. My doctor said I was lucky I didn’t have a stroke. Now I eat one cup. One. Cup. Every other day. And I cry. Not because I’m sad - because I miss my green monster smoothies. 🥲
Sara Stinnett
January 5, 2026 AT 23:58Warfarin is a relic of 20th-century medicine - a band-aid on a bullet wound. The real problem is that pharmaceutical companies profit from lifelong monitoring, not cures. DOACs are better, yes - but they’re also 20x more expensive. So we keep people on warfarin not because it’s best, but because it’s profitable. Wake up.
linda permata sari
January 7, 2026 AT 22:23I’m from Indonesia and my uncle took warfarin after his valve replacement. He said the hardest part wasn’t the bleeding - it was the stares when he told people he couldn’t eat nasi goreng because of the soy sauce and turmeric. He cried. Not from pain. From loneliness. We need more compassion in medicine.
Brandon Boyd
January 8, 2026 AT 23:30Hey, you’re not alone. I was scared too. But every time I checked my INR and saw it was in range, I felt like I won a tiny battle. You’re not just surviving - you’re mastering your body. Keep going. You’ve got this.