CNS Depressant Interactions: Risks, Common Drugs, and How to Stay Safe
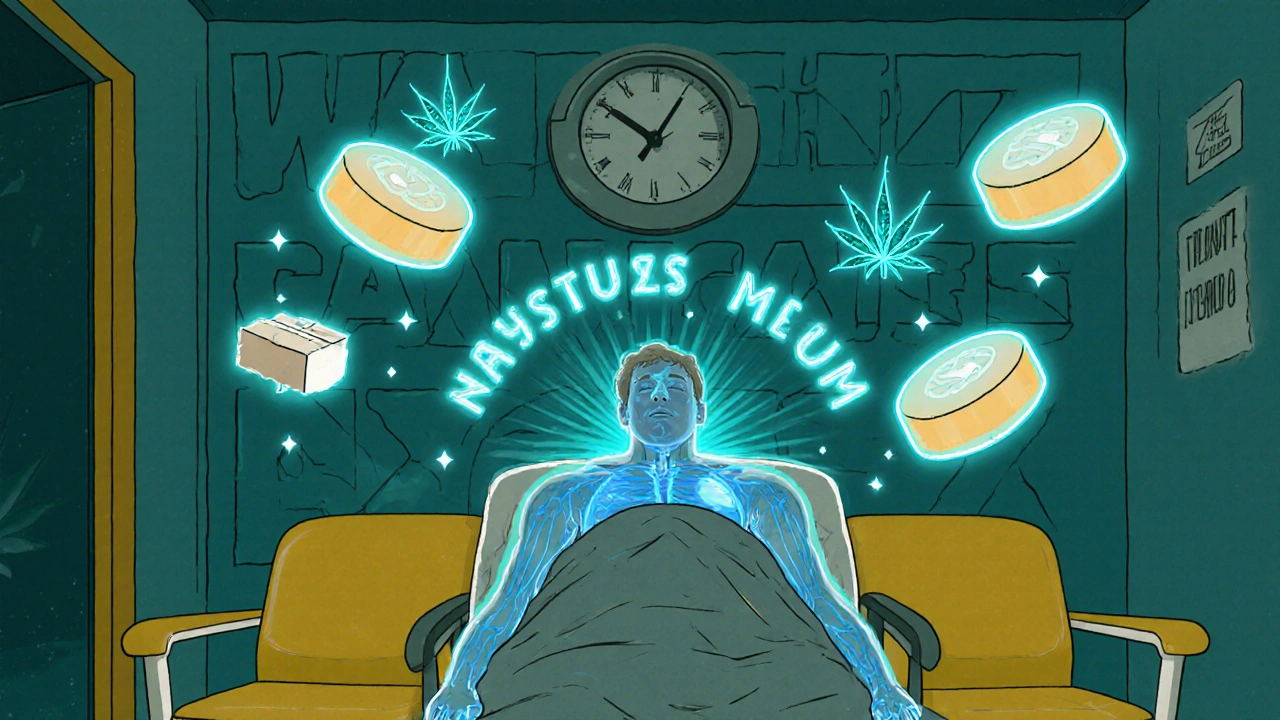
When you take a CNS depressant, a type of drug that slows down brain activity to reduce anxiety, induce sleep, or control seizures. Also known as central nervous system suppressants, it includes medications like benzodiazepines, barbiturates, sleep aids, and opioids. Mixing these with other depressants—like alcohol, certain painkillers, or even some antihistamines—can slow your breathing to a dangerous level, or worse.
These interactions aren’t rare. People often don’t realize that a sleep pill combined with a muscle relaxant or a painkiller with wine can create a silent emergency. The body doesn’t distinguish between prescription and recreational substances when it comes to CNS depression—it just adds up the effects. That’s why someone taking oxycodone for back pain and alprazolam for anxiety might feel fine one day and struggle to breathe the next. Even over-the-counter sleep aids containing diphenhydramine can become risky when paired with antidepressants or anti-anxiety meds. The risk isn’t just about dosage—it’s about combinations you didn’t think mattered.
Some of the most common and dangerous pairings involve benzodiazepines, a class of drugs used for anxiety, insomnia, and seizures, including diazepam, lorazepam, and clonazepam, and opioids, pain relievers like morphine, hydrocodone, and fentanyl that also depress breathing. When these two are taken together, the chance of fatal respiratory failure jumps dramatically. Alcohol, even in small amounts, acts like a third depressant on top of that. And it’s not just about illegal use—many people mix these without knowing, because their doctor prescribed one and they grabbed a bottle of wine or a cold medicine without checking.
You don’t need to be a heavy user to be at risk. Even someone taking one prescribed CNS depressant and accidentally adding another—like a nighttime allergy pill with diphenhydramine—can slip into danger. Older adults are especially vulnerable because their bodies process these drugs slower, and they’re more likely to be on multiple prescriptions. The symptoms aren’t always obvious: dizziness, extreme drowsiness, confusion, slurred speech, or trouble staying awake. If you or someone you know starts acting unusually sleepy after starting a new med or mixing substances, it’s not just "feeling tired"—it could be a warning sign.
What you’ll find in the posts below are real, practical guides from people who’ve dealt with these risks firsthand. You’ll see how to spot dangerous combinations before they happen, what to ask your pharmacist when picking up a new script, and how to set up safety checks so you never accidentally double-dose on depressants. There are stories about managing pain without stacking opioids, using sleep aids without alcohol, and recognizing when a medication change puts you at risk. This isn’t theory—it’s what happens when people stop guessing and start asking the right questions.