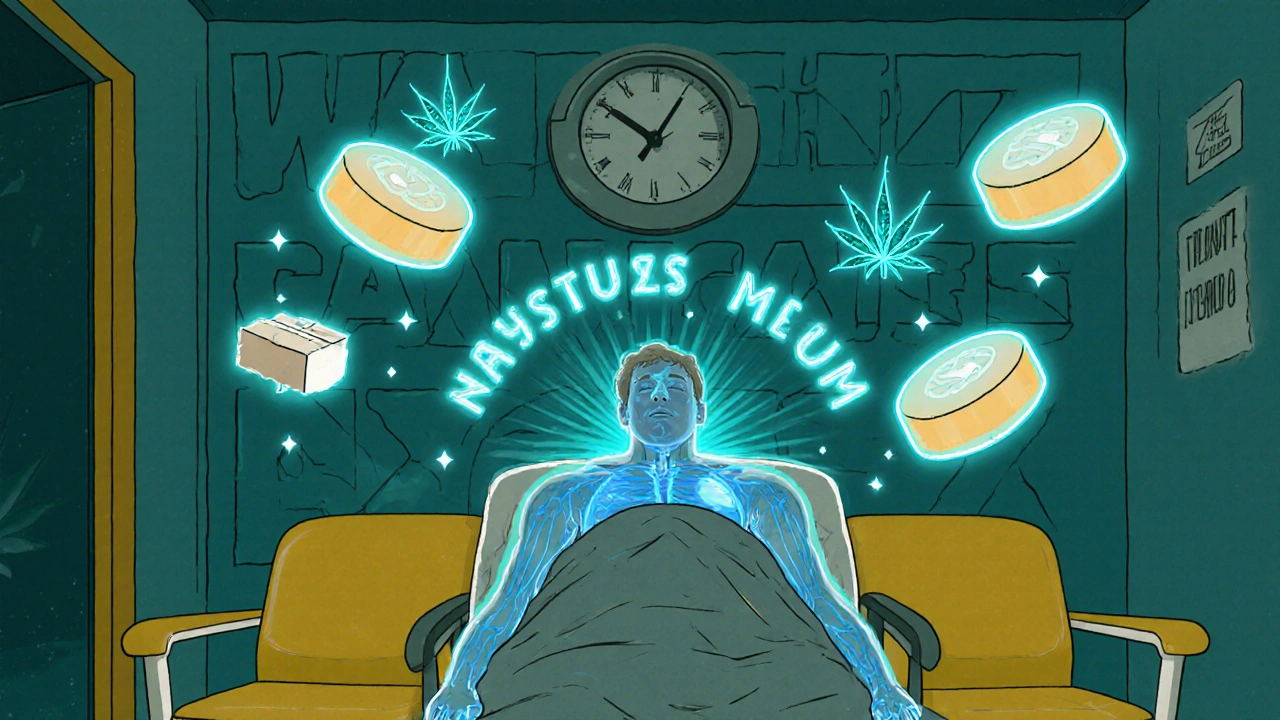
Cannabis Respiratory Depression: Risks, Signs, and What You Need to Know
When people talk about cannabis respiratory depression, a condition where breathing slows dangerously due to cannabis use, often in combination with other depressants. It's not common on its own, but it becomes a real concern when mixed with opioids, alcohol, or benzodiazepines. Most users won’t experience it—especially with isolated THC or CBD—but the risk spikes when multiple substances are involved. This isn’t theoretical. Emergency rooms see cases where people overdosed after combining cannabis with prescription painkillers or sedatives. The body’s natural breathing control gets suppressed, and without help, oxygen levels drop fast.
Opioid interaction, the combined effect of cannabis and opioids on the brainstem’s respiratory center is the biggest red flag. Studies show that while cannabis alone rarely causes fatal breathing issues, it can amplify the respiratory depression caused by opioids like oxycodone or fentanyl. The same goes for alcohol—drinking while using cannabis increases sedation and lowers the threshold for breathing problems. Even people who think they’re "just relaxing" with a joint and a beer might be putting themselves at risk. This is why emergency guidelines now warn against mixing these substances, especially in high doses or for those with existing lung or heart conditions.
Respiratory suppression, the medical term for slowed or shallow breathing caused by CNS depressants doesn’t always come with obvious signs at first. You might feel unusually drowsy, have trouble staying awake, or notice slow, irregular breaths. Loved ones often spot it first—labored breathing, blue lips, or unresponsiveness. If you or someone you know uses cannabis regularly and takes other medications, it’s worth checking if any of them are CNS depressants. Even over-the-counter sleep aids or antihistamines can add up.
Some people assume cannabis is completely safe because it’s natural. But natural doesn’t mean harmless when combined with other drugs. The real danger isn’t the cannabis itself—it’s the unseen interactions. That’s why understanding your full medication list matters. If you’re using cannabis for pain, anxiety, or sleep, talk to your doctor about what else you’re taking. You don’t need to quit cannabis, but you do need to know the risks.
Below, you’ll find real, practical guides on managing drug interactions, spotting side effects before they turn dangerous, and choosing safer alternatives when needed. Whether you’re using CBD for inflammation, THC for sleep, or just curious about how cannabis affects your body, these posts give you the facts—not the hype.