Sleep Apnea and Respiratory Failure: How Oxygen Therapy and CPAP Work Together
 Dec, 23 2025
Dec, 23 2025
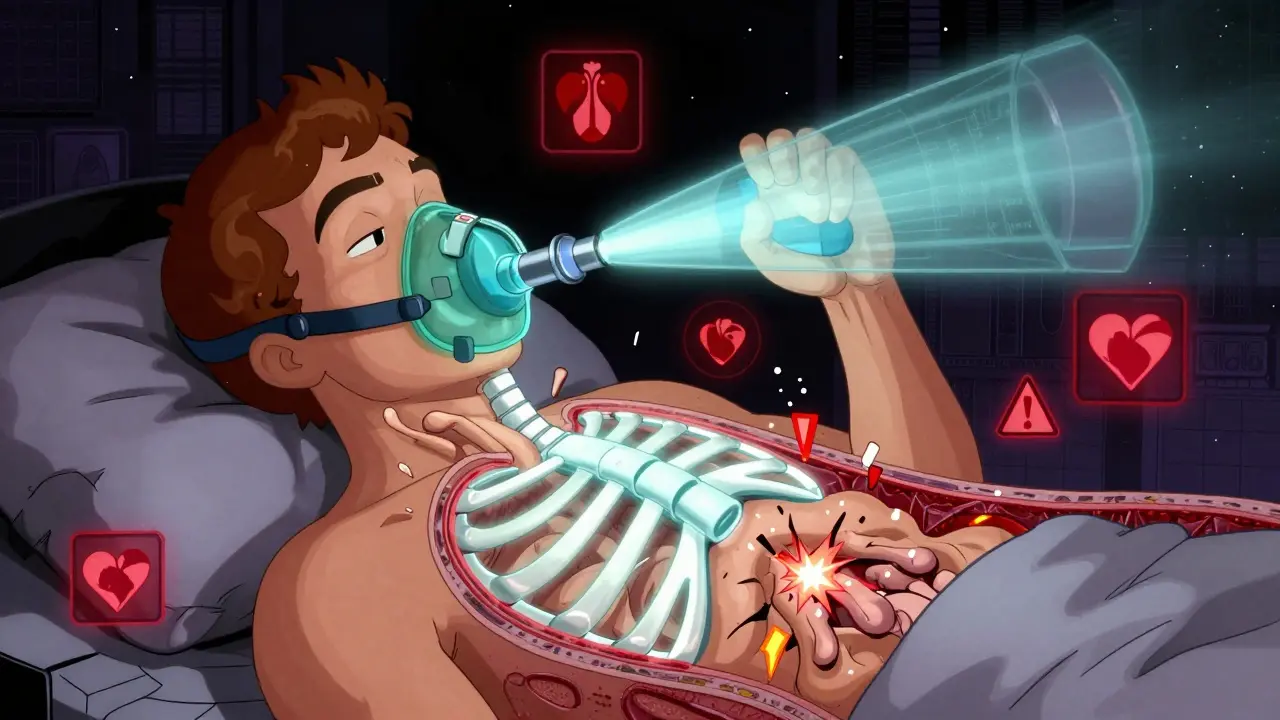
When your breathing stops repeatedly during sleep, your body doesn’t just feel tired-it’s struggling to survive. Sleep apnea isn’t just snoring. It’s a dangerous condition where your airway collapses, oxygen levels drop, and your heart works harder just to keep you alive. Left untreated, it can lead to respiratory failure, where your lungs can’t get enough oxygen or remove enough carbon dioxide. For millions, the solution isn’t surgery or pills-it’s a simple machine that blows air into your nose while you sleep. But not everyone understands how it works, or why oxygen alone isn’t enough.
What Happens When You Stop Breathing in Your Sleep?
In obstructive sleep apnea (OSA), the muscles in your throat relax too much during sleep. Your tongue and soft tissues collapse backward, blocking your airway. Each blockage lasts 10 seconds or longer, sometimes hundreds of times a night. Your brain jolts you awake just enough to breathe again-without you even realizing it. This cycle fragments your sleep and starves your body of oxygen.Over time, this repeated hypoxia (low oxygen) strains your heart, raises your blood pressure, and increases your risk of stroke, heart attack, and irregular heart rhythms. Studies show people with untreated severe OSA have a 30% higher risk of heart disease than those without it. And when OSA gets bad enough, your body can’t keep up-even when you’re awake. That’s when respiratory failure kicks in: your lungs fail to maintain safe oxygen and carbon dioxide levels.
Why Oxygen Therapy Alone Doesn’t Fix Sleep Apnea
Many assume giving extra oxygen will solve the problem. After all, if your blood oxygen drops, shouldn’t more oxygen help? It does-temporarily. Supplemental oxygen can raise your SpO2 levels during the night, but it doesn’t touch the root cause: the blocked airway.Think of it like trying to fill a balloon with a hole in it. Oxygen therapy adds air, but the leak stays open. Your body still wakes up repeatedly. Your sleep stays broken. Your blood pressure doesn’t drop. Your heart still gets hammered. That’s why the American Thoracic Society and the American Academy of Sleep Medicine say oxygen therapy should never be used alone for OSA. It’s a band-aid, not a cure.
How CPAP Actually Works-And Why It’s the Gold Standard
Continuous Positive Airway Pressure (CPAP) doesn’t give you extra oxygen. It gives you pressure. A small machine pushes a steady stream of air through a mask, keeping your throat open like a pneumatic splint. The air pressure acts like a brace, holding your airway open so you can breathe normally-even when you’re asleep.Since its invention in 1981, CPAP has become the most effective treatment for moderate to severe OSA. When used correctly, it reduces apnea events by 90%. That means instead of 30-40 breathing pauses per hour, you’re down to fewer than 5. Your oxygen levels stabilize. Your sleep deepens. Your body finally gets the rest it needs.
CPAP machines work at pressures between 4 and 20 cm H₂O, adjusted to your needs. Most people use a nasal mask (73% of users prefer it), nasal pillows, or a full-face mask if they breathe through their mouth. Modern devices include heated humidifiers to prevent dryness-something 73% of users say makes a huge difference in comfort.
CPAP vs. Other Treatments: What Actually Works
There are alternatives, but few match CPAP’s effectiveness. Mandibular advancement devices (MADs)-oral appliances that push your jaw forward-help mild to moderate OSA. But for severe cases, CPAP reduces apnea events twice as much. A 2023 review found CPAP cut the apnea-hypopnea index (AHI) to under 5 in 90% of compliant users. MADs only did it in about half.For central sleep apnea (CSA)-where your brain doesn’t send the right breathing signals-CPAP often fails. That’s where adaptive servo-ventilation (ASV) comes in. ASV adjusts pressure based on your breathing pattern, reducing central events by 68%. But ASV is dangerous for people with severe heart failure. The SERVE-HF trial showed it increased death risk in those patients. So, knowing the type of sleep apnea you have matters.
And now, there’s a new option: the hypoglossal nerve stimulator (Inspire). It’s a small implant that stimulates the nerve controlling your tongue, preventing it from blocking your airway. In a 2023 trial, 79% of patients stuck with it after a year-much higher than CPAP’s typical 50% adherence rate. But it’s expensive, requires surgery, and isn’t for everyone.
Adherence Is the Real Challenge
CPAP works-but only if you use it. And here’s the problem: nearly half of people quit within the first year. Why? Mask discomfort, dry mouth, claustrophobia, and noise. One Reddit user summed it up: “It felt like sleeping with a jet engine strapped to my face.”But success stories are common too. A survey of 12,500 CPAP users found 68% felt more alert within two weeks. Those who got in-person setup help had 32% higher adherence than those who did everything remotely. Simple fixes help: chin straps for mouth breathers, humidifiers for dryness, and gradually increasing pressure over a few nights.
Insurance companies now require proof of use-4+ hours per night, on 70% of nights-to keep covering the device. But experts say that’s not enough. The real goal is not just hours used, but whether your AHI stays under 5 and your oxygen levels stay above 90%. A 2022 study showed patients who met these physiological targets had far fewer hospital visits and better heart health.
When CPAP Isn’t Enough: Respiratory Failure and NIV
In advanced cases-especially with COPD or heart failure-OSA can lead to acute respiratory failure. Your body can’t clear carbon dioxide. Your blood turns acidic. That’s when CPAP isn’t enough. You need non-invasive ventilation (NIV), which delivers two levels of pressure: higher when you inhale, lower when you exhale. This is called BiPAP.NIV reduces the need for intubation by 20-30% in COPD flare-ups. If your blood pH doesn’t improve within 1-4 hours of starting NIV, your risk of death rises sharply. A 2021 study found patients who didn’t respond within 6 hours had 28% higher 30-day mortality than those who improved sooner.
That’s why doctors don’t just hand you a CPAP machine and say “use it.” They monitor you. They check your blood gases. They adjust pressure. They follow up at 72 hours and again at 30 days. Sleep centers that use multidisciplinary teams-respiratory therapists, sleep specialists, nurses-see 22% higher adherence than those that don’t.
What’s Changing in 2025?
Technology is catching up to the adherence problem. New CPAP machines now track your usage, mask leaks, and even your breathing patterns in real time. ResMed’s AirView platform cuts follow-up visits by 27% because doctors can spot issues remotely. Medicare pays $209.74 per month for CPAP, but insurers now demand proof of use before renewing coverage.The FDA reclassified CPAP devices to Class III in 2021 after Philips recalled 3.5 million machines due to toxic foam breakdown. That means stricter safety checks. And in 2024, the American Academy of Sleep Medicine will update guidelines to move beyond the “4-hour rule.” They’ll start measuring success by how you feel-your energy, your blood pressure, your sleep quality-not just how long you wore the mask.
What You Need to Do Right Now
If you’ve been diagnosed with sleep apnea:- Don’t accept oxygen therapy as your only treatment-it doesn’t fix the blockage.
- Give CPAP a real shot. Use it every night, even if it feels weird at first.
- Ask for a heated humidifier and a mask that fits well. Try different types until one feels comfortable.
- Get in-person help for setup. Telemedicine is convenient, but face-to-face fitting boosts adherence by over 30%.
- Track your symptoms. If you’re still tired after two weeks, your pressure may need adjusting.
- If you have heart failure or COPD, make sure your doctor checks for central apnea or respiratory failure before prescribing CPAP.
Sleep apnea isn’t a lifestyle issue. It’s a medical emergency disguised as snoring. CPAP isn’t perfect-but it’s the most proven tool we have to keep you breathing, sleeping, and alive. The goal isn’t to wear a mask forever. It’s to wake up feeling like yourself again.

Blow Job
December 24, 2025 AT 18:07I used to think CPAP was for old folks with snoring problems until I started blacking out at my desk. After three months of using it, I went from barely functioning to running 5Ks. It’s not glamorous, but it’s the difference between surviving and living.
Stop making excuses. Your future self will thank you.
Christine Détraz
December 26, 2025 AT 03:30My husband refused CPAP for two years. Said it felt like a prison. Then one night he woke up gasping, called 911, and spent three days in the ER. Now he uses it every night with a humidifier and a silly cartoon mask he picked out himself. He says it’s the best thing he ever bought-even if it looks like a sci-fi prop.
It’s not about how it looks. It’s about waking up without your heart trying to escape your chest.
Bhargav Patel
December 27, 2025 AT 04:37The philosophical underpinning of modern sleep medicine reveals a profound paradox: we treat symptoms with technology while neglecting the existential condition of modern life that renders rest itself a luxury.
CPAP, though clinically efficacious, functions not merely as a therapeutic device but as a symbolic artifact of our alienation from natural rhythms. We have engineered a mechanical solution to a biological crisis born of urbanization, screen saturation, and the commodification of rest.
One must ask: if the body is starved of oxygen due to collapsible airways, is the true pathology not merely anatomical, but cultural? The machine restores breath, but not peace. The machine restores rhythm, but not meaning.
And yet-we cannot deny its grace. In a world that demands constant wakefulness, the quiet hum of a CPAP is a lullaby of resistance.
Perhaps the true cure lies not in replacing the mask, but in relearning how to sleep without fear.
Charles Barry
December 27, 2025 AT 11:27They don’t want you to know this, but CPAP machines are part of a $12 billion sleep-industrial complex designed to keep you dependent. The foam in those Philips machines? Toxic. The FDA knew. The manufacturers knew. They just waited until the warranty expired.
And oxygen therapy? That’s what they give you to shut you up while they sell you the $3,000 machine. Your ‘doctor’ is just a sales rep with a stethoscope.
Real solution? Sleep on your side. Stop eating carbs. Quit alcohol. But no, they’d rather bill your insurance for a machine that makes you feel like you’re sleeping inside a vacuum cleaner.
Wake up. They’re not helping you. They’re selling you a prison with a warranty.
Rosemary O'Shea
December 28, 2025 AT 17:33How quaint. A 1981 invention still the gold standard? How utterly predictable. The fact that we still rely on a noisy, uncomfortable contraption to do the job of basic physiology speaks volumes about the stagnation of medical innovation.
Meanwhile, in Europe, they’ve been using AI-driven nasal dilators and biofeedback sleep patches for years. But no-Americans cling to their $3,000 jet engines because ‘it’s proven.’
Proven to be a status symbol for the sleep-deprived middle class, perhaps. But not a triumph of medicine. More like a tragic compromise.
Joe Jeter
December 29, 2025 AT 10:27Everyone’s acting like CPAP is the answer. But have you considered that maybe your body just doesn’t want to sleep? Maybe the problem isn’t your airway-it’s your life. Your job. Your anxiety. Your phone. Your Netflix addiction.
What if you’re not supposed to sleep 8 hours? What if evolution didn’t design us for this? What if the real cure is turning off the lights and going to bed at 9 PM… like our grandparents did?
CPAP doesn’t fix your insomnia. It just lets you keep living your 3 a.m. scrolling life while pretending you’re healthy.
Sidra Khan
December 30, 2025 AT 02:27CPAP is the most overhyped thing since the Segway 😅
My sister used it for 3 weeks then threw it in the garage. Said it felt like breathing through a wet sock while a dragon sat on her chest. Now she just sleeps with a pillow between her knees and calls it a day.
Also, why is everyone acting like oxygen therapy is a scam? My grandma’s on it and she’s 89 and still knitting sweaters. Maybe it’s not perfect, but it’s better than nothing.
Lu Jelonek
December 30, 2025 AT 06:19In Japan, they’ve developed a lightweight, bamboo-fiber mask that reduces pressure points and integrates with ambient sound therapy. It’s not widely available in the U.S. because insurance reimbursement models don’t account for culturally adapted design.
Also, many East Asian populations have naturally narrower airways, which is why traditional CPAP masks often don’t fit well. The one-size-fits-all approach ignores biological diversity.
There’s a reason adherence rates are higher in countries where clinicians work with patients to customize-not just prescribe.
Joseph Manuel
December 30, 2025 AT 11:11It is imperative to clarify that the assertion regarding oxygen therapy as a mere ‘band-aid’ is not entirely without merit, yet it risks oversimplification. In patients with comorbid COPD and OSA (overlap syndrome), supplemental oxygen remains a critical component of nocturnal management, even alongside CPAP.
Moreover, the claim that CPAP reduces apnea events by 90% is based on idealized, controlled trial conditions. Real-world adherence and efficacy are significantly lower, and the variability in mask interface design, pressure titration, and patient compliance renders generalizations misleading.
Furthermore, the absence of longitudinal data on long-term neurological outcomes following CPAP use necessitates caution in declaring it a definitive solution.
Medical practice requires nuance, not dogma.
Harsh Khandelwal
December 31, 2025 AT 20:06Yo, I read this whole thing and still think it’s all a scam. CPAP? Nah. I just sleep with a tennis ball sewn into my pajama back and boom-no more snoring. I’ve been doing it for 5 years. No machine, no $3K debt, no weird air pressure feeling like my face is in a wind tunnel.
And yeah, I know the docs say it’s ‘not medically proven’-but I’m alive, ain’t I? My wife says I still snore a little, but she says it’s ‘charming’ now. So maybe the real problem isn’t my throat… it’s her ears.
Also, I heard the FDA banned CPAP foam because it turns into carcinogenic glitter. That’s wild. You think they’re hiding the truth? I think they’re scared we’ll figure out sleep is just a capitalist illusion.
Spencer Garcia
January 1, 2026 AT 23:34I was skeptical too. First week: hated it. Second week: still hated it. Third week: I slept through the night for the first time in 10 years. No more morning headaches. No more falling asleep at red lights.
Try the nasal pillows. Get the humidifier. Ask for a ramp setting. Don’t give up before you’ve given it 30 days.
You don’t need to love the machine. You just need to let it help you breathe.