Methadone and QT Prolongation: Essential ECG Monitoring Guidelines
 Feb, 13 2026
Feb, 13 2026
Methadone QT Prolongation Risk Calculator
Risk Factors
Your treatment recommendations will appear here after calculation
When someone starts methadone for opioid dependence, the focus is often on recovery - fewer cravings, less illicit drug use, and a chance to rebuild life. But hidden beneath that progress is a quiet, potentially deadly risk: methadone can stretch out the heart’s electrical cycle, leading to a condition called QT prolongation. Left unchecked, this can trigger a chaotic, life-threatening heart rhythm called Torsades de Pointes. It’s rare, but it happens. And unlike an overdose, it doesn’t come with warning signs like slowed breathing. It just… stops.
Why Methadone Affects the Heart
Methadone works by binding to opioid receptors in the brain, but it doesn’t stop there. It also blocks a specific potassium channel in heart cells called hERG (human ether-a-go-go-related gene). This channel, controlled by the KCNH2 gene, is responsible for letting potassium flow out of heart cells during the final phase of each heartbeat. When that flow is blocked, the heart takes longer to reset after each beat. That delay shows up on an ECG as a longer QT interval.This isn’t just theory. Studies show methadone can lengthen the QT interval by 12 to 42 milliseconds - enough to push some people into dangerous territory. The effect isn’t linear; it doesn’t always get worse with higher doses, but it often does. People on doses over 100 mg per day are at noticeably higher risk. And when you add other factors - like low potassium, older age, or another QT-prolonging drug - the risk multiplies.
What’s a Normal QT Interval?
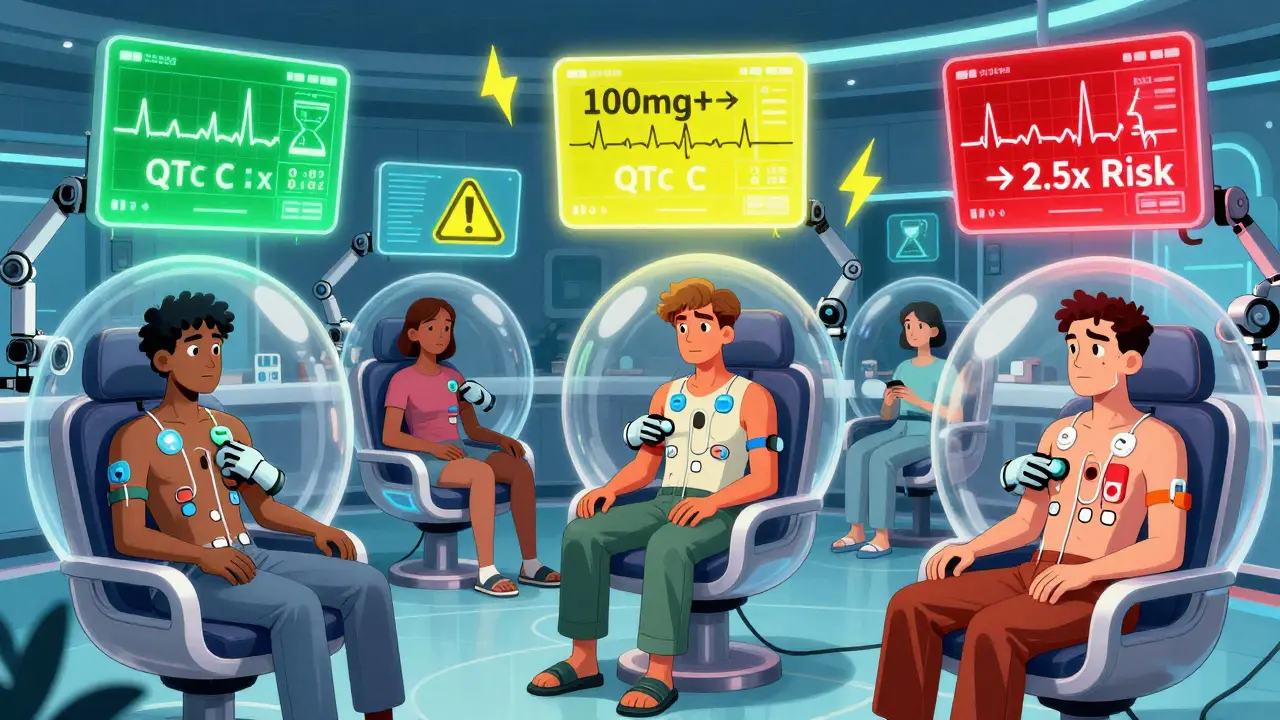
Not all QT prolongation is the same. Doctors use a corrected value, called QTc, to account for heart rate. Here’s what matters:- Normal: ≤430 ms for men, ≤450 ms for women
- Borderline: 431-450 ms for men, 451-470 ms for women
- Significant prolongation: >450 ms for men, >470 ms for women
- High risk: >500 ms (risk of sudden death jumps 4-fold)
These numbers aren’t arbitrary. Data from the University of Rochester Medical Center and Medsafe show that once QTc hits 500 ms, the chance of Torsades de Pointes rises sharply. Even a rise of more than 60 ms from baseline is a red flag - even if the absolute number hasn’t crossed 500 yet.
Who’s at Highest Risk?
Not everyone on methadone needs monthly ECGs. Risk isn’t one-size-fits-all. The biggest danger signs are:- Female gender: Women have 2.5 times higher risk than men - even at the same dose.
- Age over 65: Older hearts don’t handle drug effects as well.
- Low potassium or magnesium: Potassium under 3.5 mmol/L or magnesium under 1.5 mg/dL dramatically increases risk.
- Heart problems: History of heart failure, low ejection fraction, or prior heart attack.
- Slow heart rate: Bradycardia under 50 beats per minute.
- Other QT-prolonging drugs: Antidepressants like amitriptyline, antipsychotics like haloperidol, or antibiotics like moxifloxacin.
- Drug interactions: Medications that slow methadone breakdown - like fluconazole, voriconazole, or fluvoxamine - can spike methadone levels by up to 50%.
One study of 127 patients in a Swiss hospital found that 28% had QT prolongation. But the real kicker? The top three predictors were: methadone dose >100 mg/day, potassium <4 mmol/L, and taking psychotropic meds. All three are common in this population. That’s not coincidence - it’s a perfect storm.
When and How to Monitor
The good news? Monitoring works. A 2023 study in JAMA Internal Medicine showed that clinics with structured ECG protocols cut serious cardiac events by 67%. Here’s how to do it right:- Baseline ECG: Do one before starting methadone - no exceptions. Even if the dose is low.
- Steady-state ECG: Repeat after 2-4 weeks. That’s when methadone levels stabilize.
- Follow-up schedule:
- Low risk: QTc under 450 (men) or 470 (women), no other risk factors → every 6 months
- Moderate risk: QTc 450-480 (men) or 470-500 (women), or 1-2 risk factors → every 3 months
- High risk: QTc over 480 (men) or 500 (women), or 3+ risk factors → every month
- When to act: If QTc >500 ms OR increases by more than 60 ms from baseline, reduce the dose, check electrolytes, and refer to cardiology. Consider switching to buprenorphine - it has far less QT risk.
Some clinics skip monitoring because it’s “too much hassle.” But data from Reddit forums shows that 82% of patients who got regular ECGs felt safer - compared to just 47% who didn’t. Trust matters. And safety isn’t optional.
What About Buprenorphine?
If someone has multiple risk factors - especially if they’re female, over 65, or already on other QT-prolonging drugs - buprenorphine is a safer alternative. It doesn’t significantly block hERG channels. Studies show its QT prolongation risk is minimal. It’s not a perfect fit for everyone (some people need higher doses than buprenorphine can provide), but for those at high cardiac risk, it’s often the better choice.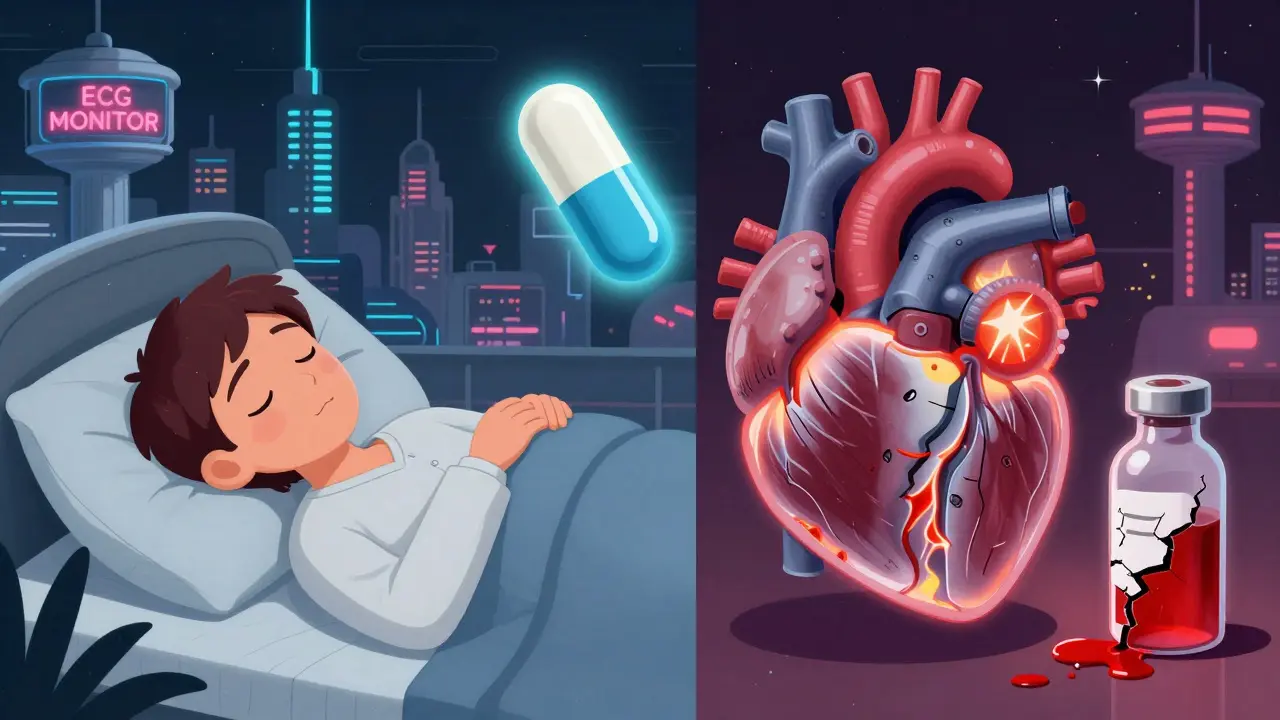
Don’t Ignore Sleep Apnea
Here’s something rarely talked about: about half of people on methadone have undiagnosed sleep apnea. That means their oxygen drops during sleep. Hypoxia stresses the heart, makes arrhythmias more likely, and can worsen QT prolongation. If someone’s on methadone and snores loudly or feels exhausted during the day, get them tested. Treating sleep apnea isn’t just about energy - it’s about preventing sudden death.Underreporting Is a Silent Crisis
The FDA has logged 142 confirmed cases of Torsades de Pointes linked to methadone since 2000. But experts believe that’s just the tip of the iceberg. In many cases, sudden death in someone on methadone is assumed to be an overdose. No autopsy. No ECG review. No recognition of cardiac arrest as the cause. That means the real number could be 3-5 times higher. Until we start treating cardiac death in this population with the same seriousness as overdose, we’re missing the full picture.Bottom Line: Monitor. Don’t Guess.
Methadone saves lives. But it can also end them - quietly, without warning. The answer isn’t to stop using it. The answer is to know who’s at risk, check their ECG at the right times, and act when the numbers tell you to. A simple 12-lead ECG, done at baseline and repeated based on risk, can prevent a death no one saw coming. In a world where addiction treatment is already stigmatized, the last thing we need is for someone to die because their heart wasn’t monitored.Do all patients on methadone need an ECG?
Yes. A baseline ECG is recommended for every patient before starting methadone. Even if the starting dose is low, it establishes a personal baseline. If the QTc is normal and there are no other risk factors, follow-up may be less frequent. But skipping the first ECG means you have no way to track changes.
Can a single ECG catch all the risk?
No. Methadone’s effect on the heart builds over time, and risk factors like electrolyte shifts or new medications can appear after treatment starts. A single ECG gives a snapshot, but ongoing monitoring is essential - especially for those on higher doses or with other risk factors. Monthly or quarterly checks are not overkill - they’re lifesaving.
What if the clinic doesn’t have an ECG machine?
Many methadone clinics partner with local hospitals or labs for ECG services. If your clinic can’t do it, they should refer you to a nearby facility. Patient safety can’t wait. If a clinic refuses to arrange ECGs, it’s a red flag. You have the right to safe care - and that includes cardiac monitoring.
Is QT prolongation reversible?
Yes. In most cases, if the methadone dose is reduced, electrolytes are corrected, and interacting drugs are stopped or switched, the QT interval will return to normal over days to weeks. The key is catching it early. Once Torsades de Pointes develops, it becomes a medical emergency.
Can I still take methadone if I have a long QT interval?
It depends. If your QTc is borderline or mildly elevated (450-480 ms for men, 470-500 ms for women) and you have no other risk factors, you may continue with close monitoring. If it’s above 500 ms or you have multiple risk factors, dose reduction or switching to buprenorphine is strongly advised. The goal isn’t to deny treatment - it’s to make it safer.
What should I ask my doctor about QT risk?
Ask: "What’s my current QTc?" "Have you checked my potassium and magnesium?" "Am I on any other meds that could increase this risk?" "How often will I need another ECG?" "Is buprenorphine an option if my risk goes up?" If they can’t answer these clearly, seek a second opinion.

Brad Ralph
February 14, 2026 AT 11:46So methadone’s basically a silent heart assassin with a recovery pamphlet. 🤡
One day you’re rebuilding your life, next you’re a human ECG spike. Guess we’re all just one potassium drop away from becoming a medical footnote.
christian jon
February 14, 2026 AT 19:46THIS IS WHY WE NEED TO STOP LETTING PEOPLE TAKE DRUGS WITHOUT A LICENSE!!
Someone’s heart is literally stretching like taffy because some clinic didn’t check a single number?!
It’s not just negligence-it’s a moral failure! Where are the police?! The FDA?!
And don’t even get me started on how buprenorphine is being pushed like it’s some miracle cure-
it’s just Big Pharma’s way of making you pay MORE for less! I’ve seen it! They swap one drug for another and call it progress!
Meanwhile, sleep apnea? HA! That’s just the tip of the iceberg-did you know the government secretly codes cardiac arrests as overdoses to hide the real death toll?!
It’s all connected. The clinics, the labs, the FDA-they’re all in on it!
And don’t tell me ‘trust your doctor’-your doctor’s paid by the same system that’s killing us!
Wake up, people! This isn’t medicine-it’s a controlled experiment on the poor!
Someone needs to sue. Someone needs to burn it all down.
And yes-I said it. I’m not sorry.
Suzette Smith
February 15, 2026 AT 06:47Honestly, I think the real issue is that we treat methadone like it’s this scary monster instead of just a tool.
People get so scared of QT prolongation that they forget it’s manageable-and often reversible.
I’ve seen folks on 120mg for years with no issues because they got their K+ checked monthly.
It’s not about fear-it’s about consistency.
Also, sleep apnea? YES. So many people just shrug off snoring. It’s not ‘just old age’-it’s a silent killer that makes everything worse.
Just… check your numbers. It’s not hard.
Autumn Frankart
February 16, 2026 AT 20:41They say ‘monitor your QT’ like it’s a suggestion.
What they don’t tell you is that half the clinics don’t even have ECG machines.
And the ones that do? They charge $300.
Meanwhile, the government gives $10,000 to a hospital to ‘study addiction’ but won’t fund a $500 ECG machine for a methadone clinic.
And you think this is about health?
No. This is about control.
They want you dependent-on the drug, on the system, on the paperwork.
They don’t want you well. They want you compliant.
And if you die quietly? Well, that’s just statistics.
They’ll say ‘it was an overdose’ and move on.
Wake up. This isn’t medicine. It’s surveillance with a stethoscope.
Pat Mun
February 17, 2026 AT 23:02I’ve been on methadone for 7 years now, and honestly? I didn’t even know about QT prolongation until last year when my nurse sat me down and said, ‘Hey, let’s get your ECG done.’
It was scary at first-I thought I was going to die tomorrow.
But then she showed me my numbers, explained what normal looked like for me, and we made a plan.
Now I get checked every 3 months, my potassium is stable, and I even started doing yoga to help my breathing.
It’s not about being perfect-it’s about being aware.
And honestly? That’s the biggest gift this program gave me: awareness.
I used to feel like a number. Now I feel like someone who’s worth checking on.
So if you’re reading this and you’re scared? You’re not alone.
And you don’t have to be scared alone.
Ask for help. Ask for the ECG. Ask for the potassium test.
You deserve to be safe.
You deserve to live.
And yes-I cried when I saw my QT drop from 490 to 440.
It was the most hopeful moment of my recovery.
andres az
February 19, 2026 AT 10:10hERG blockade is a pharmacokinetic red herring.
the real issue is CYP3A4/2D6 polymorphism heterogeneity in the population.
most clinicians lack the bioinformatics literacy to interpret QTc drift in context of polypharmacy.
also, potassium levels are not linearly predictive-there’s a threshold effect at 3.2 mmol/L with non-parametric variance.
and buprenorphine? please. its partial agonism profile introduces its own arrhythmogenic risk via beta-adrenergic modulation.
we need longitudinal ECG-omics datasets with real-time telemetry.
until then, this is all anecdotal noise wrapped in clinical jargon.
Steve DESTIVELLE
February 20, 2026 AT 23:27People think medicine is about science
But it is about power
Who decides what is safe
Who decides who gets monitored
Who decides if your heart matters
They call it treatment
But it is control
They give you methadone
But take your freedom
They say monitor your QT
But they do not monitor their own greed
The system does not care if you live
It only cares if you obey
And when you die quietly
They will say you were at risk
As if that was enough
As if that was justice
It is not science
It is silence
And silence is the loudest lie
Stephon Devereux
February 21, 2026 AT 05:31One thing I wish more people understood: QT prolongation isn’t a failure-it’s a signal.
It’s not that methadone is ‘dangerous’-it’s that our systems aren’t designed to support high-risk patients.
But here’s the good news: we can fix this.
Baseline ECGs? Free in most states under Medicaid.
Electrolyte panels? Often covered with zero copay.
Cardiology referrals? Many clinics have partnerships with local hospitals.
And buprenorphine? It’s not a ‘last resort’-it’s a valid first option for high-risk folks.
Most people don’t know these options exist because no one told them.
So if you’re reading this and you’re scared? Ask your provider: ‘What’s my plan?’
Not ‘Is this safe?’
But ‘What’s my plan?’
Because if you have a plan-you’re already ahead of 80% of patients.
And that? That’s power.
Reggie McIntyre
February 22, 2026 AT 04:03Just got my QTc checked yesterday-442 ms. Felt like winning the lottery.
Three years ago, I was at 488. I didn’t even know what that meant.
Now I know my potassium needs to be above 4.0, I avoid azithromycin like the plague, and I actually talk to my pharmacist about interactions.
It’s wild how much changes when you stop treating your body like a mystery box.
Also-sleep apnea test? Best thing I ever did. No more 3pm naps. No more heart pounding at night.
Turns out, breathing matters.
Who knew?
Jack Havard
February 23, 2026 AT 17:03They say ‘monitor your QT’ but never mention that 70% of the time, the machine is broken or the tech doesn’t know how to interpret it.
Also, who’s paying for these monthly ECGs? Because if you’re on Medicaid in Alabama, good luck.
And buprenorphine? Sure, it’s ‘safer’-but it’s also harder to get and requires weekly visits.
So what’s the real goal here? Safety-or control?
And why does no one talk about how these rules hit Black and rural communities the hardest?
It’s not medicine.
It’s a gatekeeping system dressed in a lab coat.
Kristin Jarecki
February 25, 2026 AT 00:25It is imperative to underscore that the implementation of standardized electrocardiographic monitoring protocols for patients receiving methadone maintenance therapy is not merely a clinical best practice-it is an ethical imperative grounded in the principles of beneficence and nonmaleficence.
Failure to establish baseline and periodic QTc assessments constitutes a deviation from the standard of care as delineated by the American Heart Association and the Substance Abuse and Mental Health Services Administration.
Furthermore, the concomitant evaluation of serum electrolytes and a comprehensive medication reconciliation must be considered integral components of this protocol, as their absence significantly elevates the risk of adverse cardiac events.
It is incumbent upon healthcare institutions to allocate necessary resources toward this end, as the cost of inaction far exceeds the cost of prevention.
Patients deserve not only the opportunity for recovery, but also the assurance of safety during that journey.
Complacency is not an option.
It is our solemn duty to act.