How to Implement a Personal Safety Checklist for Pharmacy Visits
 Jan, 26 2026
Jan, 26 2026
Every year, thousands of people in the UK get the wrong medicine at the pharmacy-not because the pharmacist made a careless mistake, but because no one double-checked. You might think pharmacies have systems to catch errors, and they do. But those systems aren’t perfect. And if you’re taking multiple medications, have a chronic condition, or just had a recent change in your prescriptions, the risk goes up. The truth? You’re the last line of defense. No checklist from a hospital or regulatory body will hand you a ready-made tool. But you can build one. Here’s how.
Start with your medication list
Before you even walk into the pharmacy, you need a current, accurate list of everything you take. Not just the big ones. Not just the pills. Include vitamins, supplements, herbal remedies, and even over-the-counter painkillers. Write down the name, dose, how often you take it, and why. Keep this list on your phone and in your wallet. Update it every time your doctor changes something.Why? Because pharmacists rely on this information to spot dangerous interactions. If you tell them you take aspirin daily but forget to mention your fish oil supplement, they might miss a bleeding risk. If you say you’re on metformin but don’t mention the new blood pressure pill your cardiologist just prescribed, they won’t know to check for kidney strain. Your list isn’t just helpful-it’s essential.
Ask for the prescription label to be read aloud
When you get your medicine, don’t just grab the bag and go. Wait. Ask the pharmacist to read the label out loud-just like they do for the elderly or visually impaired. It’s not a weird request. It’s standard practice in safe pharmacies.Listen carefully. Compare what they say to your own list. Does the name match? Is the dose the same? Is the frequency correct? If they say “take one tablet twice daily” but your doctor wrote “once daily,” speak up. You’d be surprised how often the printed label is wrong. A 2022 study in the British Journal of Clinical Pharmacology found that 1 in 12 prescription labels had at least one error-wrong dose, wrong frequency, or wrong patient name. You’re not being difficult. You’re being smart.
Check the physical pill or liquid
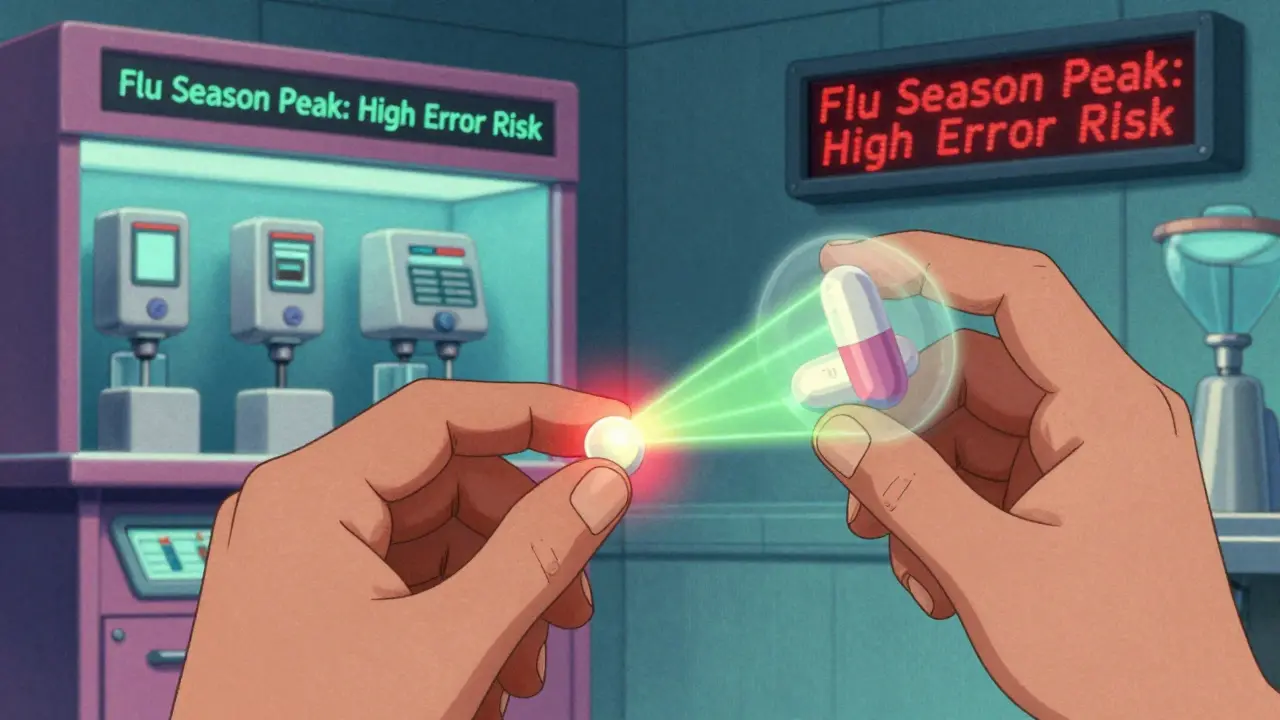
Look at the medicine in your hand. Does it look right? If you’ve been taking the same pill for months and suddenly it’s a different color, shape, or has a different imprint, ask about it. Generic drugs can look different from brand names, but they should still match the description on the label.For liquids, check the color and smell. If your insulin looks cloudy when it should be clear, or your antibiotic syrup smells sour instead of sweet, don’t take it. Pharmacists can make mistakes when filling prescriptions-especially under pressure. A 2023 report from the National Patient Safety Agency found that 27% of dispensing errors occurred during high-volume periods like flu season. Your eyes are a backup system.
Confirm the reason for the medicine
Ask: “Why am I taking this now?” If the pharmacist says, “It’s for your blood pressure,” but you haven’t been diagnosed with high blood pressure, something’s off. If they say, “This is a refill of your last antibiotic,” but you finished it two weeks ago and didn’t get a new prescription, question it.Medication errors often happen because of miscommunication between doctors and pharmacies. Maybe your doctor changed your prescription but didn’t send the update. Maybe the pharmacy pulled the wrong file. Either way, you’re the only one who knows what you were actually prescribed. Don’t assume it’s right. Confirm it.
Use the ‘teach-back’ method
After the pharmacist explains how to take the medicine, repeat it back to them in your own words. Say: “So, I take this one with food every morning, and I shouldn’t drink grapefruit juice while on it, right?” If they correct you, listen. If they say, “Yes, that’s right,” you’ve just created a safety checkpoint.This technique, called the teach-back method, is used in hospitals to reduce readmissions. It works for pharmacies too. A 2021 trial in NHS pharmacies showed that patients who used teach-back had 40% fewer medication errors in the first week after a new prescription. It’s simple. It’s effective. And it’s free.
Keep a visit log
After every pharmacy visit, write down three things: the date, the medicine you received, and any changes the pharmacist mentioned. Keep it in a notebook or a notes app on your phone. Include the name of the pharmacist if you remember it. This creates a paper trail.Why? Because if something goes wrong later-like you feel dizzy after starting a new pill-you’ll have proof of what you were given. You might need it if you have to talk to your doctor, file a complaint, or even report a potential error to the Medicines and Healthcare products Regulatory Agency (MHRA).

Know your red flags
Some signs mean something’s seriously wrong. Don’t ignore them:- The pharmacy gives you a medicine you’ve never heard of, and they can’t explain why.
- The bottle has someone else’s name on it-even a similar name.
- The dosage is way higher than what your doctor prescribed.
- The pill looks completely different from your last refill, and they can’t explain why.
- You’re handed a controlled drug (like oxycodone or diazepam) without any counseling.
If any of these happen, don’t leave without asking for the pharmacist in charge. If you’re still not satisfied, call your doctor’s office. Or go to another pharmacy. Better safe than sorry.
Build your personal checklist
Here’s your simple, printable checklist. Keep it in your wallet or on your phone:- I have my current medication list with doses and reasons.
- I ask the pharmacist to read the label out loud.
- I compare the pill or liquid to my last refill.
- I confirm why I’m taking this medicine.
- I use the teach-back method to repeat instructions.
- I write down what I received and any changes.
- I walk away if something feels wrong.
Use this every time. Even if you’ve been going to the same pharmacy for 10 years. Even if you trust the staff. Because mistakes happen to everyone-even the best pharmacies.
What if you spot an error?
If you catch a mistake, don’t panic. Say: “I think there might be an error. This doesn’t match my prescription.” Most pharmacists will thank you. They’re trained to fix errors. If they dismiss you, ask to speak to the manager. If they still don’t help, file a report with the General Pharmaceutical Council (GPhC). You can do it online. It takes five minutes. And it could stop someone else from getting the wrong medicine.Remember: You don’t need to be a medical expert to protect yourself. You just need to be observant, curious, and willing to speak up. The system isn’t perfect. But you can be the missing piece.

Josh josh
January 27, 2026 AT 04:27Karen Droege
January 27, 2026 AT 08:04shivam utkresth
January 27, 2026 AT 23:22Angie Thompson
January 28, 2026 AT 20:38Shweta Deshpande
January 30, 2026 AT 10:25Aishah Bango
January 30, 2026 AT 15:49Robin Van Emous
January 31, 2026 AT 09:01SWAPNIL SIDAM
February 1, 2026 AT 16:51bella nash
February 1, 2026 AT 20:24