How Medicare Part D Generics Save Money on Copays in 2026
 Jan, 18 2026
Jan, 18 2026
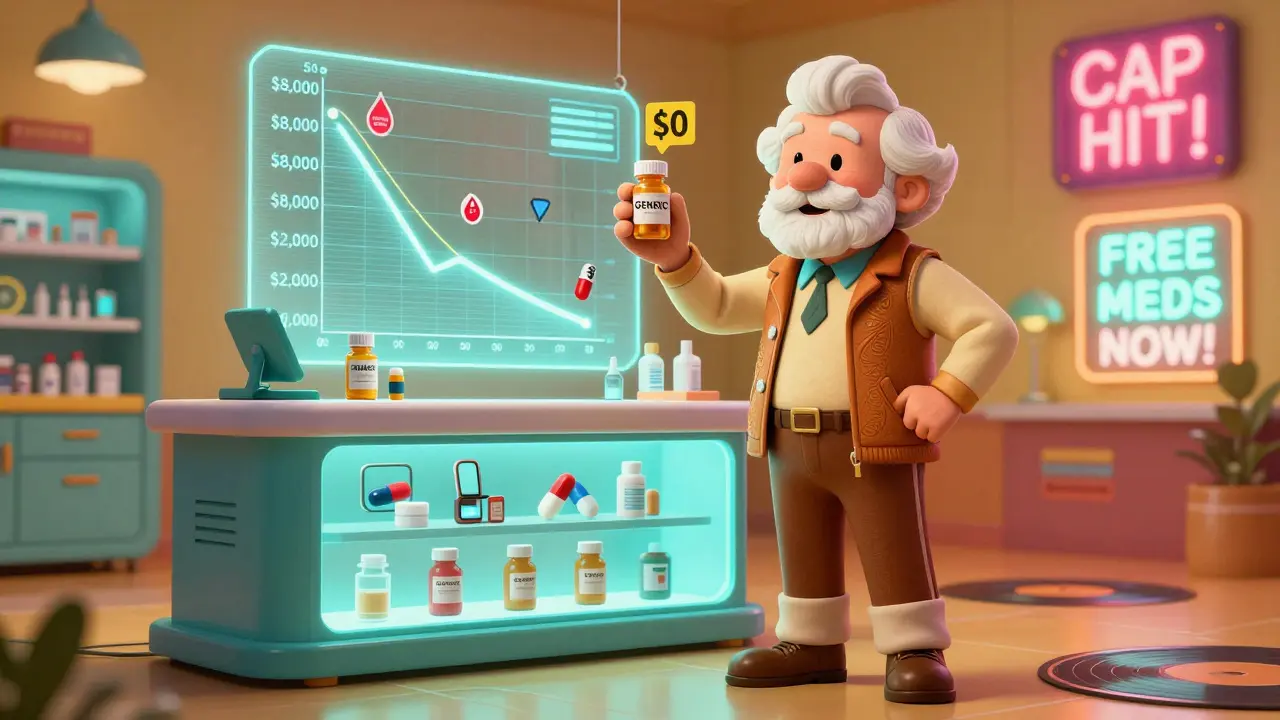
By 2026, if you're on Medicare and take generic drugs, your out-of-pocket costs could be dramatically lower than just a few years ago. The changes to Medicare Part D under the Inflation Reduction Act aren't just paperwork-they're putting real money back in your pocket. For millions of seniors and people with disabilities, the biggest win isn't a new brand-name drug. It's the fact that your $10 generic blood pressure pill now costs you $0 after you hit a $2,000 annual cap on what you pay out of pocket. That’s not a guess. That’s the law, and it’s in effect.
What Changed in Medicare Part D for Generics?
Before 2025, Medicare Part D had a coverage gap, often called the "donut hole." If you took multiple generic medications, you could spend thousands of dollars before hitting catastrophic coverage. Some beneficiaries paid nearly $8,000 out of pocket before their costs dropped. That’s not a typo. Eight thousand dollars. Now, thanks to the Inflation Reduction Act, the out-of-pocket cap for all Part D drugs-brand or generic-is $2,000 per year. Once you hit that number, you pay nothing for the rest of the year. That includes all your generics. No more coinsurance. No more surprise bills. Just $0 copays. This cap applies to what’s called "true out-of-pocket" (TrOOP) spending. That means your deductible, copayments, and coinsurance all count. But your monthly premium doesn’t. And here’s a key detail: manufacturer discounts on generics also count toward your $2,000 cap. That’s new. Before, those discounts didn’t help you reach the cap. Now they do.How Much Do Generics Actually Cost Under Part D?
Most Medicare Part D plans put generics on the lowest tier of their formulary, meaning they’re the cheapest option. In 2025 and 2026, the median copay for a 30-day supply of a preferred generic is about $10. That’s the same whether you’re in a stand-alone Part D plan or a Medicare Advantage plan with drug coverage. But here’s where it gets even better. If you’re enrolled in a Part D plan with a deductible, you’ll pay that first. In 2026, the maximum deductible is $590. After that, you pay 25% of the drug’s cost until you hit $2,000. For a $10 generic, that’s just $2.50 per prescription after the deductible. Many people never even reach the deductible because their monthly meds are so cheap. And if you qualify for Extra Help (Low-Income Subsidy), your costs drop even further. You pay $0 deductible and $0 to $4.50 per generic prescription. No cap needed. No waiting. Just low, predictable costs.Part D Plans vs. Medicare Advantage: Which Saves More?
You might think all Part D plans are the same. They’re not. There are two main types: stand-alone Prescription Drug Plans (PDPs) and Medicare Advantage Prescription Drug plans (MA-PDs). PDPs are separate from your Medicare coverage. You pay a monthly premium-on average $39 in 2025. That’s a lot. But your generic copays are still around $10. MA-PDs bundle your Medicare Part A, Part B, and drug coverage into one plan. The average monthly premium for the drug portion? Just $7. That’s a huge difference. And your copays for generics? Still $10. So if you’re taking mostly generics, you’re saving on premiums and copays at the same time. The real savings? It’s not just about what you pay per pill. It’s about what you pay over the year. If you take five generics a month at $10 each, you’re spending $600 a year. With the $2,000 cap, you’d hit that limit in under 34 months. After that, your meds are free. That’s why many people say, "I used to pay $1,200 a year for my meds. Now I pay $0."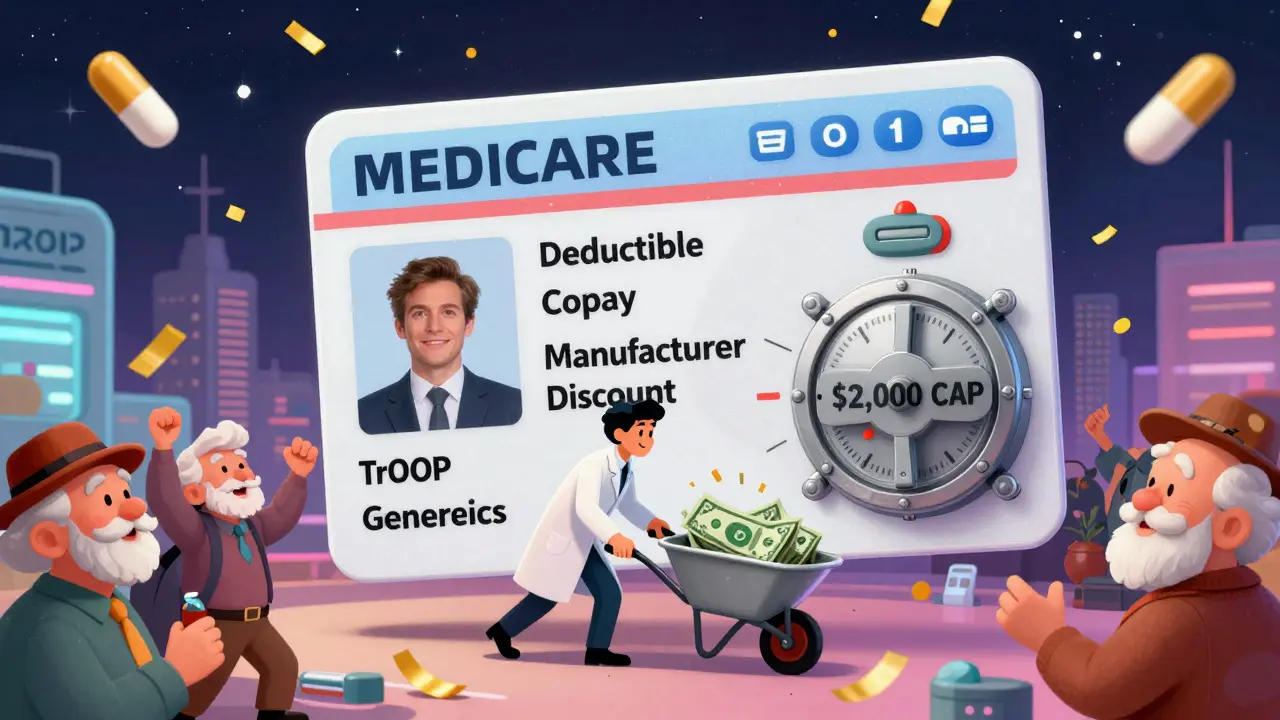
Why Some People Still Struggle With Generic Coverage
It’s not all smooth sailing. Even with the $2,000 cap, many beneficiaries still face roadblocks. One big issue is formulary changes. Insurance companies can swap out one generic version of a drug for another-even if they’re the same strength and dosage. That’s called therapeutic substitution. If your plan switches from a $5 generic to a $12 generic, your copay jumps. And you might not find out until you go to pick up your prescription. Another problem? Prior authorization. Even for generics, some plans require you to get approval before they’ll cover the drug. That’s rare with generics, but it’s happening more than it should. The Accessible Medicines Foundation found Part D plans use prior authorization on generics more than private insurance plans do. Then there’s the confusion around the $2,000 cap. A KFF study in 2024 found that 41% of beneficiaries didn’t understand how manufacturer discounts counted toward their out-of-pocket limit. If you think your $10 copay is the only thing that counts, you’re wrong. The discount the drugmaker gives the plan? That counts too. And that can help you reach the cap faster.How to Make Sure You’re Getting the Best Generic Coverage
You don’t have to guess. You can check your plan’s coverage every year during Open Enrollment (October 15 to December 7). Use the Medicare Plan Finder tool. Type in your exact medications-generic names, dosages, how often you take them. The tool shows you exactly what you’ll pay at each pharmacy. Look for plans that list your drugs on Tier 1. That’s the cheapest tier. Check if your plan uses step therapy. That means you have to try a cheaper generic first before they’ll cover another. If you’ve been on a certain generic for years and your plan suddenly requires you to switch, that’s a red flag. If you’re on Extra Help, make sure you’re enrolled. You might qualify even if you didn’t before. Income limits are higher now. You can apply through Social Security or your state Medicaid office. And if you’re still paying more than $2,000 a year for your meds, you’re not doing something right. The cap is automatic. You don’t have to apply for it. Once you hit $2,000, your plan should switch you to $0 copays. If it doesn’t, call your plan. Ask them to review your TrOOP spending.

Erwin Kodiat
January 19, 2026 AT 16:58This is the kind of policy change that actually matters. I’ve been watching my dad’s copays drop since last year-he takes five generics, and now he just laughs when the pharmacist says, "Your total is $0." No more skipping doses. No more choosing between meds and groceries. It’s not magic. It’s just smart legislation.
And yeah, the $2,000 cap? It’s automatic. No forms. No applications. Just hit the number and breathe easy. If your plan isn’t doing it, call them. They’re supposed to track TrOOP. If they don’t, complain until they fix it.
Also-don’t let anyone tell you Medicare Advantage is worse. My cousin’s MA-PD has a $7 premium and same $10 generics. She saves more than I do on my standalone Part D. It’s not about the plan type-it’s about the drug tier and the cap.
Valerie DeLoach
January 19, 2026 AT 22:12I’ve spent the last decade helping seniors navigate Part D, and I can tell you-this is the first time in my career that the math actually works in the patient’s favor. The $2,000 cap isn’t a perk; it’s a moral correction.
What’s more, the inclusion of manufacturer discounts in TrOOP? That was a quiet revolution. Before, drugmakers gave discounts, but the beneficiary never saw the benefit. Now, those discounts push people faster toward $0 copays. That’s not just policy-it’s justice.
And for those worried about formulary swaps? You’re right to be. But the Plan Finder tool lets you compare exact drug tiers. Use it. Don’t assume your plan is still the same. Open Enrollment isn’t optional-it’s your lifeline.
Jake Rudin
January 21, 2026 AT 15:35Let’s be clear: the Inflation Reduction Act didn’t just cap costs-it exposed the entire pharmaceutical pricing structure as a fraud. Generics have been priced at $10 for decades, yet insurers and PBMs kept extracting $8 of that as profit. Now? The cap forces transparency. The discounts count. The system can’t hide anymore.
And yet-why are we still talking about $10 copays? Why aren’t we demanding $0 at the counter, regardless of cap? Why is the system still built on a threshold? Why not just eliminate all cost-sharing for generics entirely? It’s not just about affordability-it’s about dignity.
Also, prior authorization on generics? That’s not oversight. That’s bureaucratic cruelty. A pill that costs 20 cents to produce shouldn’t require a 3-day approval process. It’s absurd.
And yes-I know some people think this is socialism. But socialism? No. This is just common sense. If you’re paying for a drug with your taxes, why are you still getting billed for it? It’s illogical. And illogical systems collapse. This one’s just beginning to.
Malikah Rajap
January 22, 2026 AT 18:59Did you know that some plans are still charging copays even after you hit the $2,000 cap? I had a friend who had to call her plan 11 times before they fixed it. They claimed it was a "system error." System error? No. It’s negligence. They know the law. They just don’t want to pay the difference.
And if you’re on Extra Help? Don’t assume you’re safe. I had a woman in my support group who was denied because her state Medicaid office didn’t update her income records. She was making $1,000 over the limit-by $18. She had to file an appeal. Don’t let bureaucracy rob you of your meds.
Also-why do pharmacies still charge $10 for generics? The wholesale cost is $0.50. The cap hides that. We should be pushing for direct price transparency. Not just caps. Real prices.
And yes-I know I sound like a nag. But someone has to. Nobody else will.
Tracy Howard
January 22, 2026 AT 22:57Canada’s system is laughably simple: generics cost $5 CAD, full stop. No caps. No tiers. No confusing TrOOP nonsense. We don’t need 2,000-page manuals to know how much we pay for insulin. We just pay $5. And we don’t have 41% of seniors clueless about how discounts work. Because it’s not complicated.
Meanwhile, you Americans turn a lifesaving policy into a labyrinth of spreadsheets and phone calls. You celebrate a $2,000 cap like it’s a gift from the gods. Meanwhile, we just... have it. No fanfare. No gratitude required.
And don’t even get me started on your "Medicare Advantage" mess. It’s not a plan. It’s a marketing brochure with hidden fees and formulary traps. You’re not saving money-you’re gambling on a plan that might drop your meds next month.
Just say it: your system is broken. The cap is a Band-Aid on a hemorrhage.
sujit paul
January 23, 2026 AT 13:29Let me ask you this: if a drug costs $0.20 to manufacture, why is the system allowing $10 copays at all? This isn’t healthcare-it’s a Ponzi scheme disguised as insurance. The cap is a distraction. It doesn’t fix the root problem: pharmaceutical monopolies, PBMs, and opaque pricing.
And you think this is progress? In India, a month’s supply of metformin costs $0.15. In the U.S., even with the cap, we’re still paying $10 because the system has no incentive to lower prices-it only has incentive to shift costs around.
The real win? Not the cap. The cap is just the first crack in the dam. The real victory is when generics cost less than a coffee. Until then, we’re just rearranging deck chairs on the Titanic.
And yes-I know you’re grateful. But gratitude without systemic change is just complicity.
Aman Kumar
January 25, 2026 AT 05:51TrOOP. Formulary tiers. Therapeutic substitution. Step therapy. Prior authorization. These are not features-they are weaponized bureaucracy. The system doesn’t want you to succeed. It wants you to navigate, to call, to appeal, to be exhausted.
And yet-you’re supposed to be thankful because you’re not paying $8,000 anymore? That’s not progress. That’s survival. We’ve normalized suffering so much that a $2,000 cap feels like a miracle.
Meanwhile, the same PBMs that profit from your copays are the ones lobbying to keep the system complex. They don’t want transparency. They want you to think it’s your fault you’re confused.
And if you’re still paying more than $2,000? You’re not failing. The system is. Call your plan. File a grievance. Document everything. Because if you don’t, they’ll keep doing this to the next person.
And no-I’m not being dramatic. I’ve seen people die because they skipped doses. This isn’t policy. It’s life or death.
Josh Kenna
January 26, 2026 AT 23:00