Clinical Outcomes Data: What Studies Reveal About Generic Medications for Providers
 Dec, 29 2025
Dec, 29 2025
When a patient walks into your office asking why they’re now taking a different pill with a different color and name, what do you say? You know the science says it’s the same drug. But patients hear "generic" and think "cheaper version"-like a knockoff handbag or a store-brand cereal. The truth is far more straightforward: generic drugs work just as well as brand-name ones for nearly every condition. And the data doesn’t just back this up-it screams it.
How We Know Generics Work the Same
The FDA doesn’t approve a generic drug just because a company says it’s similar. It requires proof. Every generic must show it delivers the same active ingredient, in the same strength, at the same rate, and in the same way as the brand-name version. That’s called pharmaceutical equivalence. But that’s only half the story. The real test is bioequivalence: does your body absorb and use the drug the same way? To prove this, manufacturers run studies with 24 to 36 healthy volunteers. They measure how much of the drug enters the bloodstream (AUC) and how fast it peaks (Cmax). The results must fall within 80% to 125% of the brand-name drug’s numbers. For most drugs, that’s enough. For narrow therapeutic index drugs-like warfarin, levothyroxine, or tacrolimus-the standards are tighter. Even then, studies show no meaningful difference in outcomes. A 2019 study in PLOS Medicine looked at over 1.3 million patients across 14 drug classes. For alendronate, glipizide, quinapril, and amlodipine, the risk of hospitalization, heart attack, or stroke was virtually identical between generics and brands. In fact, for amlodipine and amlodipine/benazepril, patients on generics had lower rates of cardiovascular events. That’s not a fluke. It’s data.What About Psychiatric Drugs? The Big Exception?
This is where things get noisy. Some studies show slightly higher psychiatric hospitalization rates with generics for escitalopram and sertraline. At first glance, that sounds alarming. But dig deeper, and the picture changes. The same study found that even when patients switched from brand-name to authorized generics-the exact same drug made by the brand company under a different label-the hospitalization rates stayed the same. That means the difference isn’t about the drug. It’s about perception. Patients who’ve been on a brand-name antidepressant for months may believe the blue capsule works better than the white one-even if they’re chemically identical. That belief can affect adherence, which then affects outcomes. It’s not the drug failing. It’s the mind playing tricks. The FDA’s own 2017 analysis found no consistent pattern of worse outcomes with generic psychiatric drugs. And when researchers controlled for patient expectations, the differences vanished.Real-World Evidence: Survival, Costs, and Switching Patterns
A 2020 study tracking 3.5 million Medicare beneficiaries found a huge gap in five-year survival rates: 85.9% for generic users versus 77.8% for brand-name users. That seems like a massive advantage for generics. But here’s the catch: the patients getting generics were healthier to begin with. They were younger. They had fewer comorbidities. They were more likely to be insured and follow up regularly. Once researchers adjusted for those factors using statistical weighting, the survival gap shrank to just 2.9 percentage points-82.7% for generics, 79.8% for brands. That’s not a drug effect. That’s a health disparity effect. And what about patients who switch back to brand-name drugs after trying generics? The FDA tracked this across 12 medications. Only 2.7% of patients on traditional generics returned to the brand. For authorized generics? Just 1.8%. Again, not because the drug failed. Because patients trusted the version they knew.
What the Experts Say
Dr. Aaron Kesselheim from Harvard Medical School reviewed 47 studies on cardiovascular drugs and found 89% showed no difference between generics and brands. The rest? Mixed results-with no clear winner. He summed it up simply: "The totality of evidence demonstrates that generic drugs are clinically equivalent to their brand-name counterparts for nearly all therapeutic classes." The American College of Physicians says it even more directly: "Physicians should generally prescribe generic drugs rather than brand-name drugs when equivalent generics are available." The FDA’s Office of Generic Drugs doesn’t mince words either: "An approved generic medicine has been shown to be bioequivalent to the brand-name medicine and is considered therapeutically equivalent." These aren’t opinions. These are conclusions based on decades of data, millions of patients, and billions of prescriptions.When Should You Be Cautious?
There are exceptions. About 3% of generic drugs are rated "B" in the FDA’s Orange Book-meaning they’re not automatically considered interchangeable. These are mostly complex formulations: inhalers, topical creams, injectables, or narrow therapeutic index drugs where tiny differences in absorption could matter. For these, you should check the Orange Book before prescribing. If a generic is rated "B," consider sticking with the brand-or at least monitor the patient closely after switching. But for the other 97%? No need to overthink it. One common concern? Appearance. Generics often look different because of inactive ingredients-dyes, fillers, coatings. Patients sometimes think a different color or shape means a different drug. But the FDA confirmed in 2019: these cosmetic differences have zero impact on how the drug works.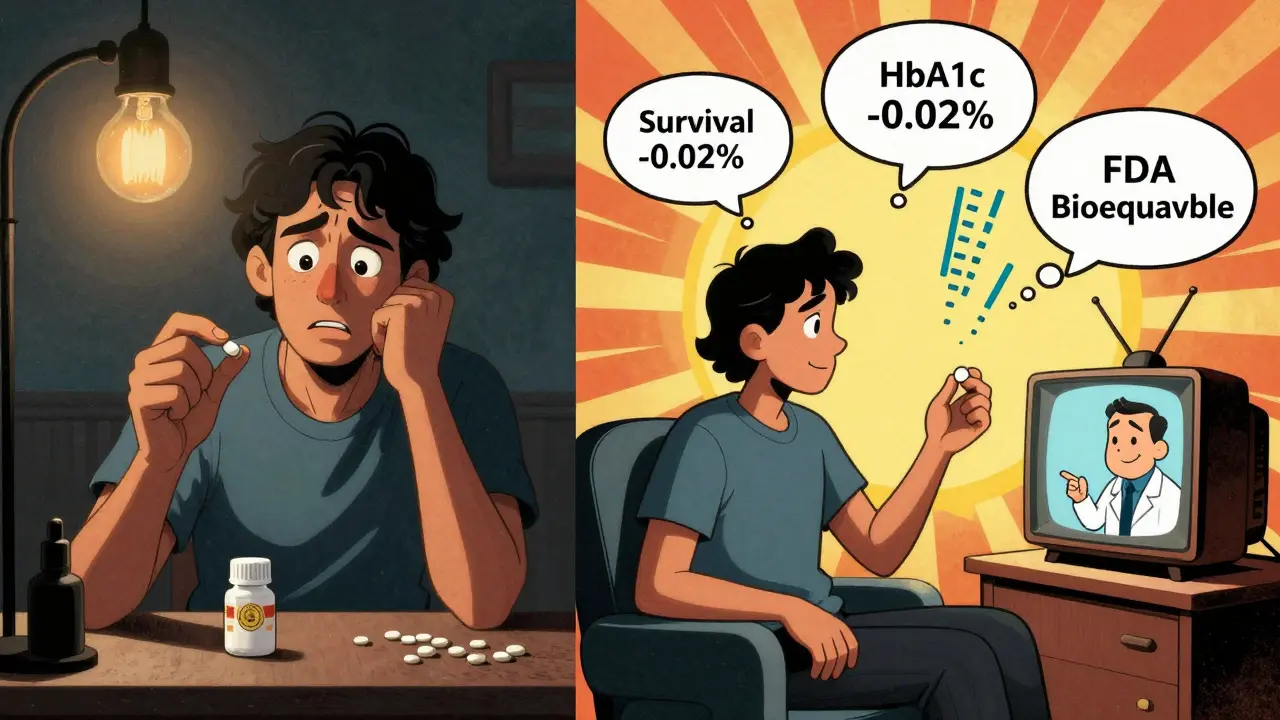
Why This Matters for Your Practice
Prescribing generics isn’t just about saving money-it’s about improving access. A patient who can’t afford their brand-name statin will skip doses. Or stop entirely. A generic version might cost $4 instead of $150. That’s not a choice. That’s survival. And the numbers don’t lie. Generics account for 90% of all prescriptions filled in the U.S. But they make up only 23% of total drug spending. From 2008 to 2017, they saved the U.S. healthcare system $1.68 trillion. In 2021 alone, they saved $377 billion. If you’re still hesitant to prescribe generics, ask yourself: Are you protecting your patient-or your comfort zone?What You Can Do Today
Start with three simple steps:- Check the FDA’s Orange Book before prescribing. Look for "A-rated" generics-those are safe to substitute.
- When switching a patient, explain why: "This is the same medicine, just cheaper. The FDA requires it to work exactly the same way."
- Address fears head-on. If a patient says, "I don’t trust the generic," ask: "What made you think it’s different?" Often, they’re just repeating what they heard. Give them facts, not jargon.
Bottom Line
You don’t need to choose between cost and care. Generics deliver both. The science is settled. The evidence is overwhelming. The savings are real. And the patients? They’re not getting second-rate medicine. They’re getting the same medicine-without the markup. Stop treating generics as a compromise. Treat them as the standard.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. Adverse event reports show only 0.02% of all drug-related safety issues involve generics, compared to 3.2% for brand-name drugs. The active ingredient is identical, and the body processes it the same way.
Why do some patients say generics don’t work for them?
Often, it’s not the drug-it’s the expectation. Patients may notice a different color, shape, or pill size and assume it’s less effective. Studies show that when patients are switched to authorized generics (made by the original brand), they still report similar concerns. This suggests the issue is psychological, not pharmacological. Education helps: explaining that the FDA requires bioequivalence can reduce anxiety and improve adherence.
Are there any drugs where generics aren’t recommended?
For most drugs, generics are equally effective. But about 3% of generics are rated "B" in the FDA’s Orange Book-meaning they’re not automatically interchangeable. These are typically narrow therapeutic index drugs (like warfarin, levothyroxine, or cyclosporine) or complex formulations (like inhalers or topical products). For these, it’s safest to stick with the brand or monitor closely after switching.
Do generics take longer to work than brand-name drugs?
No. Bioequivalence studies require generics to reach the same blood concentration levels at the same rate as the brand-name drug. The time to peak concentration (Tmax) and overall exposure (AUC) must be within strict limits. If a generic worked slower, it wouldn’t pass FDA approval.
Why are generics so much cheaper?
Generics are cheaper because they don’t need to repeat expensive clinical trials. The original brand company already proved the drug is safe and effective. Generic manufacturers only need to prove their version delivers the same amount of active ingredient the same way. That cuts development costs by 80-90%. Savings are passed on to patients and insurers.
Can I switch a patient from brand to generic safely?
For most medications, yes-with one exception: narrow therapeutic index drugs. For those, check the FDA’s Orange Book for an "A" rating. For all others, switching is not just safe-it’s standard practice. Studies show no increase in hospitalizations, emergency visits, or discontinuation rates after switching to generics. In fact, lower costs often improve adherence.

David Chase
December 31, 2025 AT 04:09This is why America is falling behind!! 🇺🇸💀 Generics? Please. I’ve seen patients on generics crash harder than my last MacBook. The FDA? More like Faux-DA. My cousin’s uncle’s neighbor took a generic statin and ended up in the ER with muscle necrosis. Yeah. It’s not coincidence. It’s corporate greed letting cheap pills slip through. 💊🔥 #StopTheGenericCon
Emma Duquemin
January 1, 2026 AT 06:01OMG YES. I’m a pharmacist in Austin and I’ve seen this play out a hundred times. Patient comes in crying because their ‘new’ antidepressant ‘doesn’t work’-turns out it’s the same exact pill, just a different shade of blue. They’re not broken. Their brain is just screaming ‘THIS ISN’T THE ONE!’ 😭💙 I start every switch with a 10-minute pep talk and a printed FDA chart. It’s wild how much placebo power lives in a pill’s color. 🎨✨
Jasmine Yule
January 3, 2026 AT 03:30David, you’re terrifying. But also… kinda right? I’ve had patients panic over generic metformin because it’s round instead of oval. Not the drug. The SHAPE. 😭 We’re not treating patients. We’re treating trauma.
Tamar Dunlop
January 4, 2026 AT 04:36As a clinician from Vancouver, I find this discussion both deeply necessary and profoundly unsettling. The emotional weight carried by patients when they are transitioned to generics is rarely acknowledged in clinical guidelines. We speak of bioequivalence as if it were a mathematical certainty-yet the human psyche, shaped by branding, advertising, and cultural narratives of quality, does not compute in equations. I have witnessed elderly patients weep upon receiving a generic version of their long-term cardiac medication, convinced they are being abandoned by the system. This is not irrationality. It is grief. And we must grieve with them, not correct them.
Sharleen Luciano
January 5, 2026 AT 00:48How quaint. You’re all acting like this is some groundbreaking revelation. The FDA’s bioequivalence standards are laughably lenient-80-125%? That’s a 45% window. In pharmacokinetics, that’s a canyon. And don’t get me started on the ‘authorized generics’ cherry-picked by lazy researchers. Real science doesn’t cherry-pick. Real science has reproducibility. And guess what? It’s missing here. 🤷♀️ This isn’t medicine-it’s marketing dressed in white coats. If you’re prescribing generics because you’re too lazy to look up the Orange Book, you’re not a healer. You’re a cost-center.
Lisa Dore
January 6, 2026 AT 03:20Sharleen, you’re brilliant but so harsh. Let’s not throw the baby out with the bathwater. Yes, the FDA’s standards aren’t perfect-but they’re the best we’ve got. And for 97% of drugs? They work. I’ve got a 72-year-old diabetic on generic metformin who’s been stable for 5 years. She saves $120/month. That’s groceries. That’s bus fare. That’s dignity. 🌱💖 Let’s fight for better standards, not against the ones that already save lives.
Greg Quinn
January 6, 2026 AT 12:52It’s funny how we treat medicine like it’s a product. But drugs aren’t cars or smartphones. They’re biochemical agents interacting with a biological system that’s as unique as a fingerprint. We quantify equivalence in AUC and Cmax, but we ignore the noise-the gut microbiome, epigenetic expression, sleep cycles, stress hormones. Maybe the ‘same drug’ isn’t the same at all. Maybe the real difference isn’t in the pill… it’s in the person taking it.
Joe Kwon
January 8, 2026 AT 08:36Agree with Greg. The bioequivalence metrics are a proxy, not a guarantee. But the population-level data is overwhelming: no increase in adverse events, no rise in hospitalizations, no drop in adherence for most drugs. The outliers? We monitor them. The rest? We optimize access. The 2.7% switch-back rate? That’s not failure-it’s human psychology. We need better patient education, not less generics. 📊🩺
Himanshu Singh
January 10, 2026 AT 05:47bro i just took a generic for my anxiety and it worked great!! i mean i thought it was gonna be weak but nope same as the brand!! i think people just overthink it like its magic or something 🤷♂️
Manan Pandya
January 12, 2026 AT 02:13As a physician in Delhi, I see this daily. In low-resource settings, generics are not a preference-they are survival. A patient choosing between insulin and rent is not choosing between quality and cost. They are choosing life. The data here mirrors the U.S.: no difference in HbA1c, no increase in ketoacidosis. The only difference? The dignity restored when a patient can afford to take their medicine every day. The science is clear. The moral imperative is clearer.
Aliza Efraimov
January 14, 2026 AT 00:40Emma’s point about the blue pill is everything. I had a patient on sertraline for 8 years. Switched to generic. Said it ‘felt different.’ We switched her to the authorized generic-same manufacturer, same pill, just different label. She cried. Said she felt ‘seen’ again. It wasn’t the drug. It was the ritual. The color. The brand. The story she told herself. We don’t treat molecules. We treat narratives. And sometimes, the narrative is the medicine.
Teresa Rodriguez leon
January 14, 2026 AT 19:03I don’t care what the data says. My sister died on a generic. She was on warfarin. The INR went wild. The hospital said it was ‘user error.’ I know better. Generics are dangerous. And you’re all just too comfortable to admit it.