DOAC Interactions with Other Medications: What You Need to Know
 Nov, 17 2025
Nov, 17 2025
Why DOAC interactions matter more than you think
If you're taking a direct oral anticoagulant (DOAC) like apixaban, rivaroxaban, dabigatran, edoxaban, or betrixaban, you might assume your blood thinner is simple to manage-no regular blood tests, fewer food restrictions, and fewer drug clashes than warfarin. That’s mostly true. But here’s the catch: DOAC interactions can still turn safe treatment into a dangerous situation. One extra pill, a new supplement, or even a common heart medication can push your drug levels too high-or too low-with life-threatening results.
Most people on DOACs are older and juggling multiple conditions. Studies show that over 80% of DOAC users take five or more other medications daily. That’s not unusual-it’s the norm. But when you mix DOACs with certain drugs, you’re not just adding another pill. You’re changing how your body handles the anticoagulant itself. Too much DOAC? Higher bleeding risk. Too little? Blood clots can form without warning.
How DOACs work-and why drugs interfere
DOACs don’t work like warfarin. Warfarin messes with vitamin K and needs constant blood tests. DOACs block specific clotting proteins directly. But their journey through your body is delicate. Two key systems control how much DOAC stays in your bloodstream: the CYP3A4 enzyme and the P-gp transporter.
Think of CYP3A4 as a factory that breaks down drugs, and P-gp as a bouncer at the cell door that decides what gets in or out. Some DOACs rely heavily on these systems:
- Apixaban: 20-25% broken down by CYP3A4, mostly cleared by P-gp
- Rivaroxaban: About half processed by CYP3A4, strongly affected by P-gp
- Dabigatran: Almost entirely handled by P-gp
- Edoxaban: Mostly cleared by P-gp
- Betrixaban: Similar to dabigatran and edoxaban
When another drug blocks or speeds up these systems, your DOAC levels swing unpredictably. A strong blocker can make your DOAC stick around too long. A strong booster can flush it out too fast. Neither is safe.
Top 5 dangerous DOAC interactions you can’t ignore
Not all drug combos are risky. But these five are well-documented, common, and can cause serious harm if missed.
1. Dronedarone (Multaq)
This heart rhythm drug is a double threat-it strongly blocks P-gp and moderately blocks CYP3A4. For dabigatran and rivaroxaban, combining them with dronedarone is a hard no. Studies show plasma levels of these DOACs can spike by over 200%. For edoxaban, the fix is simple: cut the dose to 30 mg once daily. Apixaban and betrixaban have less data, but caution is still advised.
2. Amiodarone (Cordarone)
Amiodarone is one of the most commonly prescribed heart drugs. It moderately blocks P-gp. When taken with any DOAC, it can increase bleeding risk. The NHS recommends checking for signs of bruising, blood in urine or stool, and unexplained fatigue. No dose change is officially required for apixaban or edoxaban, but many clinicians lower the DOAC dose anyway-especially in older adults or those with kidney issues.
3. Verapamil and Diltiazem
These calcium channel blockers are used for high blood pressure and angina. Verapamil weakly blocks CYP3A4 but strongly blocks P-gp. Diltiazem is similar. For dabigatran, the dose should drop to 110 mg twice daily for atrial fibrillation or clot treatment. For rivaroxaban and apixaban, the interaction is less clear. Some studies show no major change, but real-world cases still report bleeding. When in doubt, monitor closely.
4. Rifampin (Rifadin)
This antibiotic and tuberculosis drug is a powerful inducer-it speeds up CYP3A4 and P-gp. Taking rifampin with any DOAC can slash drug levels by up to 50%. That’s not a small drop. It’s enough to leave you unprotected against clots. If you need rifampin, switch to warfarin temporarily or delay DOAC use until after treatment ends.
5. St. John’s Wort
This herbal supplement is sold as a natural antidepressant. But it’s also a strong CYP3A4 and P-gp inducer. One study showed it cut rivaroxaban levels by nearly 30%. People think herbal means safe. It doesn’t. Always tell your doctor about every supplement you take-even if you bought it at the corner store.
Other risks: NSAIDs, SSRIs, and antiplatelets
Some drugs don’t change DOAC levels-but still raise bleeding risk. These are pharmacodynamic interactions: they work on the same system, just differently.
- NSAIDs (ibuprofen, naproxen): Increase stomach bleeding risk. Use acetaminophen instead if you need pain relief.
- SSRIs (sertraline, fluoxetine): Can affect platelet function. Risk is low but real, especially in older adults.
- Aspirin, clopidogrel: Often prescribed with DOACs after heart attacks or stents. Triple therapy (DOAC + aspirin + clopidogrel) is common-but doubles bleeding risk. Guidelines now recommend stopping one antiplatelet after 30 days if possible.
There’s no perfect solution. Sometimes the benefit of preventing another heart attack outweighs the bleeding risk. But it should be a conscious decision-not an accident.
Dosing matters: One size doesn’t fit all
Not all rivaroxaban doses are the same. A 20 mg once-daily dose for atrial fibrillation is different from 2.5 mg twice daily after a heart attack. The lower dose has different blood levels and clearance patterns. The same applies to dabigatran: 150 mg twice daily is higher risk for stomach bleeding than 110 mg. Edoxaban’s standard dose is 60 mg, but drops to 30 mg for people with kidney problems or those on P-gp blockers.
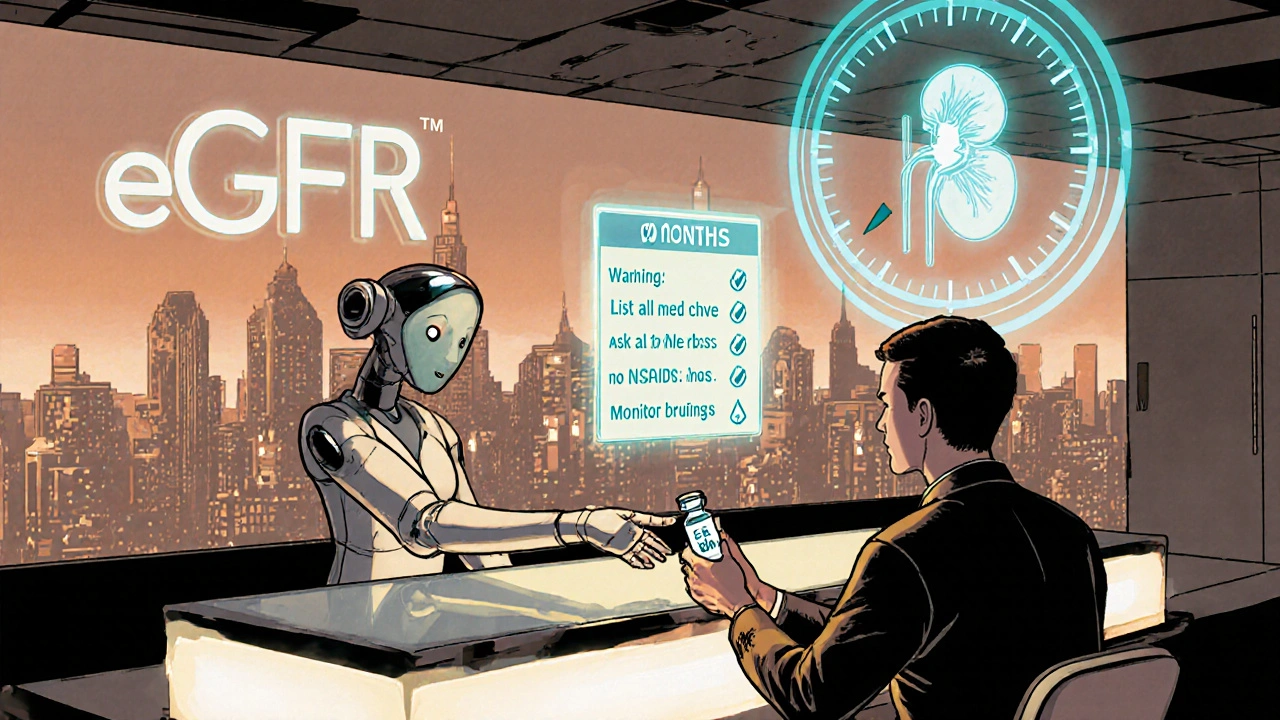
When a drug interaction occurs, you can’t just guess the fix. You need to know:
- Which DOAC you’re on
- Why you’re taking it (stroke prevention? clot treatment?)
- Your kidney function (eGFR)
- What the interaction does to drug levels
For example: Someone on 150 mg dabigatran for stroke prevention who starts verapamil should drop to 110 mg. But if that same person has kidney impairment (eGFR 30), they might already be on 110 mg-so no change is needed. Context is everything.
What to do if you’re on multiple medications
Here’s a simple action plan:
- Make a complete list of everything you take: prescriptions, over-the-counter meds, vitamins, herbs, even eye drops.
- Bring this list to every doctor visit-don’t assume they’ll ask.
- Ask your pharmacist: “Does this new drug interact with my blood thinner?” Pharmacists are trained for this.
- Watch for signs of bleeding: unusual bruising, nosebleeds, dark stools, pink or red urine, headaches with dizziness.
- Don’t stop or change your DOAC dose on your own-even if you feel fine.
Also, check your kidney function regularly. DOACs are cleared by the kidneys. If your kidneys slow down, your DOAC builds up-even without any drug interactions. A simple blood test (eGFR) every 6-12 months can catch this early.
What’s new in DOAC interaction management
Experts are pushing for more research. Right now, we’re guessing a lot. We know dronedarone and rifampin are dangerous. But what about newer drugs like apixaban with a new antidepressant? Or edoxaban with a recently approved cholesterol drug? We don’t have data.
Some researchers suggest we should start using therapeutic drug monitoring-measuring DOAC levels in the blood-to guide doses. It’s already done in hospitals for some patients. But it’s not routine. Why? Because it’s expensive, not standardized, and we don’t yet have clear “safe” ranges for every condition.
But here’s the future: personalized dosing. One day, your DOAC dose might be adjusted based on your genetics, kidney health, and other meds-not just your weight or age. Until then, vigilance is your best tool.
Bottom line: DOACs are safer-but not foolproof
Compared to warfarin, DOACs are easier to use. No weekly blood tests. Fewer food limits. But they’re not magic. Every pill you add changes the balance. Polypharmacy isn’t just a buzzword-it’s a real threat.
Don’t assume your doctor knows every interaction. Don’t assume your pharmacist will catch everything. And never assume a supplement is harmless.
The goal isn’t to avoid all meds. It’s to manage them wisely. If you’re on a DOAC and take more than five other drugs, you’re in the high-risk group. That means you need more-not less-attention.
Stay informed. Stay alert. And never stop asking questions.
Can I take ibuprofen while on a DOAC?
It’s not recommended. Ibuprofen and other NSAIDs increase the risk of stomach bleeding when taken with DOACs, even if they don’t change the drug’s level in your blood. Use acetaminophen (paracetamol) instead for pain or fever. If you must take ibuprofen, use the lowest dose for the shortest time possible-and talk to your doctor first.
Is it safe to take St. John’s Wort with apixaban?
No. St. John’s Wort speeds up how your body clears apixaban, reducing its effectiveness by up to 30%. This can leave you unprotected against clots. Even if you feel fine, your risk of stroke or deep vein thrombosis goes up. Stop the supplement and talk to your doctor before switching to another antidepressant.
What should I do if I start a new antibiotic?
Always check with your doctor or pharmacist before starting any new antibiotic. Rifampin is dangerous with DOACs and must be avoided. Other antibiotics like clarithromycin or fluconazole can also interfere. If you need an antibiotic, your DOAC dose may need to be adjusted-or you may need to switch temporarily to warfarin. Never guess.
Can kidney problems affect DOAC interactions?
Yes. DOACs are cleared by the kidneys. If your kidney function is low (eGFR below 50), your DOAC builds up in your blood even without other drugs. Adding a P-gp blocker like verapamil on top of poor kidney function can push levels dangerously high. Always get your eGFR checked at least twice a year if you’re on a DOAC.
Do I need blood tests to monitor my DOAC?
Routine blood tests aren’t needed for DOACs like they are for warfarin. But if you’re on multiple interacting drugs, have kidney issues, or have had bleeding or clotting events, your doctor might order a specific test (anti-Xa or ecarin clotting time) to check your DOAC level. This isn’t common-but it’s an option when things get complicated.
What if I miss a dose because of an interaction?
Don’t double up. If you miss a dose of apixaban or rivaroxaban, take it as soon as you remember-if it’s within 6 hours. For dabigatran or edoxaban, if it’s within 6 hours, take it. After that, skip it and take your next dose at the regular time. Never take two doses at once. If you’re unsure, call your doctor or pharmacist.

Bailey Sheppard
November 18, 2025 AT 12:24Girish Pai
November 18, 2025 AT 23:12Kristi Joy
November 19, 2025 AT 06:49Hal Nicholas
November 20, 2025 AT 11:58Louie Amour
November 20, 2025 AT 20:54Kristina Williams
November 20, 2025 AT 23:42Shilpi Tiwari
November 22, 2025 AT 22:57Christine Eslinger
November 23, 2025 AT 07:14Sarah Frey
November 23, 2025 AT 20:21