Arimidex (Anastrozole) vs Other Breast Cancer Drugs: Detailed Comparison
 Oct, 4 2025
Oct, 4 2025
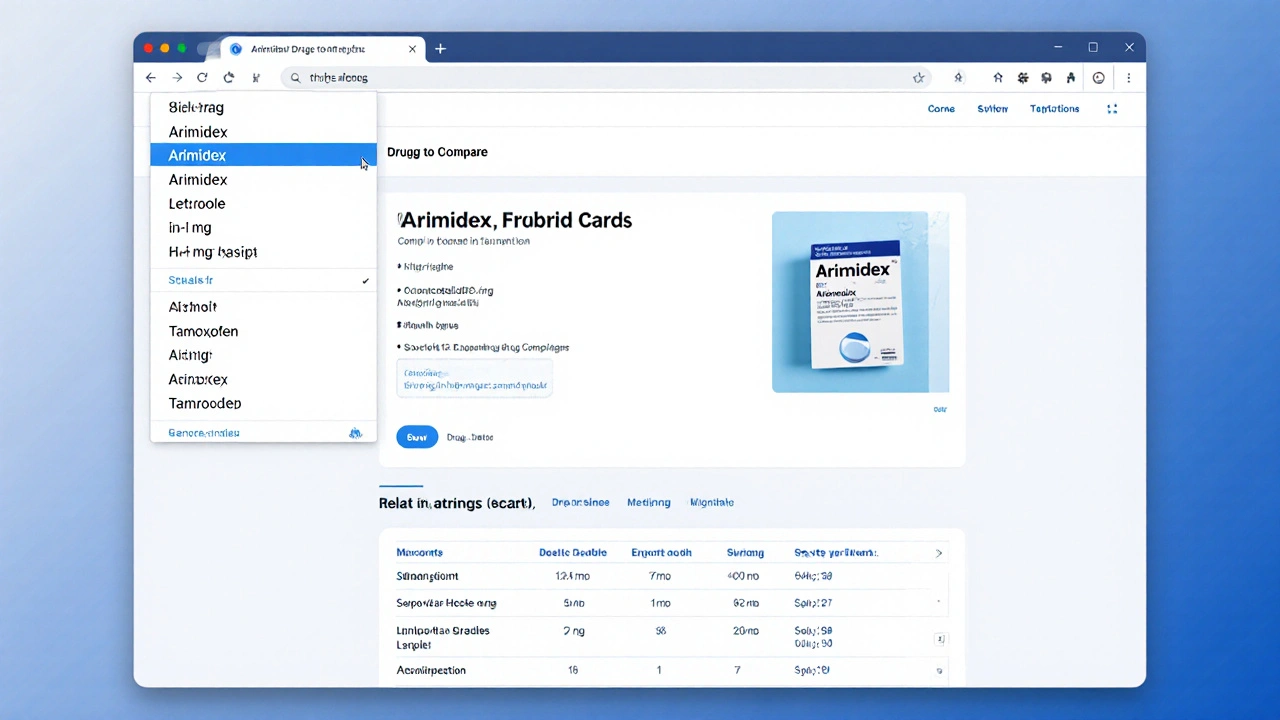
Arimidex vs Other Breast Cancer Drugs Comparison Tool
Select a drug and situation, then click "Compare Selected Drug" to see detailed information.
| Drug | Class | Dosage | Primary Advantage | Common Side Effects |
|---|---|---|---|---|
| Arimidex | Aromatase inhibitor (non-steroidal) | 1 mg PO daily | Convenient oral dosing, strong estrogen suppression | Arthralgia, hot flashes, bone loss |
| Letrozole | Aromatase inhibitor (non-steroidal) | 2.5 mg PO daily | Very high estrogen reduction, useful in neoadjuvant setting | Joint pain, fatigue, hot flashes |
| Exemestane | Aromatase inhibitor (steroidal) | 25 mg PO daily | Irreversible binding may delay resistance | Muscle aches, nausea, bone loss |
| Tamoxifen | Selective estrogen receptor modulator (SERM) | 20 mg PO daily | Effective for pre-menopausal patients, bone-preserving | Clot risk, endometrial thickening, hot flashes |
| Fulvestrant | Estrogen receptor antagonist | 500 mg IM injection | Useful after aromatase inhibitor failure | Injection site pain, nausea, liver enzyme rise |
| Goserelin | LHRH agonist | 3.6 mg SC every 28 days | Suppresses ovarian estrogen production | Menopausal symptoms, injection site irritation |
When doctors talk about hormonal therapy for estrogen‑receptor‑positive breast cancer, Arimidex vs Letrozole often pops up first. But Arimidex isn’t the only player in the room. Knowing how it stacks up against other options can save you from surprise side effects, unnecessary costs, or a therapy that just doesn’t fit your lifestyle.
Key Takeaways
- Arimidex (anastrozole) is a third‑generation aromatase inhibitor taken once daily.
- Letrozole and exemestane are the closest alternatives, with slightly different dosing and side‑effect profiles.
- Tamoxifen works on the estrogen receptor instead of blocking estrogen production, making it useful in younger patients.
- Fulvestrant and goserelin target the hormone pathway in other ways and are usually reserved for advanced or resistant cases.
- Choosing the right drug depends on age, menopausal status, comorbidities, and how your body reacts to estrogen suppression.
What is Arimidex (Anastrozole)?
Arimidex is a selective aromatase inhibitor that blocks the enzyme aromatase, preventing the conversion of androgens into estrogen. It is approved for post‑menopausal women with hormone‑receptor‑positive breast cancer and is taken as a 1mg tablet once daily. The drug was first approved by the FDA in 1995 and quickly became a standard part of adjuvant therapy because it lowers estrogen levels by about 97%.
Common Alternatives
Below are the most frequently prescribed alternatives, each with its own twist on hormone suppression.
Letrozole
Letrozole is another third‑generation aromatase inhibitor, typically dosed at 2.5mg daily. It was approved in 1997 and is known for a slightly stronger estrogen‑lowering effect than anastrozole, though clinical outcomes are largely comparable.
Exemestane
Exemestane is a steroidal aromatase inhibitor taken at 25mg daily. Unlike the non‑steroidal anastrozole and letrozole, exemestane binds irreversibly to the aromatase enzyme, which some clinicians believe may lead to fewer resistance issues.
Tamoxifen
Tamoxifen is a selective estrogen receptor modulator (SERM) that blocks estrogen receptors in breast tissue while acting like estrogen in bone and the uterus. The usual dose is 20mg daily for five years. It works for both pre‑ and post‑menopausal women, making it a versatile alternative when aromatase inhibitors aren’t suitable.
Fulvestrant
Fulvestrant is a pure estrogen receptor antagonist administered via intramuscular injection (500mg on days 0, 14, 28, then monthly). It degrades the receptor, offering a different mechanism for patients whose disease progresses on oral hormonal therapy.
Goserelin
Goserelin is a luteinizing‑hormone‑releasing hormone (LHRH) agonist that suppresses ovarian estrogen production. It is given as a subcutaneous implant (3.6mg every 28 days) and is mainly used in pre‑menopausal women.
How These Drugs Work - The Mechanistic Landscape
All the drugs above aim to starve estrogen‑dependent tumors, but they do it in three distinct ways:
- Aromatase inhibition - Arimidex, Letrozole, and Exemestane block aromatase, the enzyme that creates estrogen from androstenedione and testosterone.
- Estrogen receptor blockade - Tamoxifen and Fulvestrant sit on the receptor, preventing estrogen from binding.
- Hormone production suppression - Goserelin shuts down the ovaries’ estrogen output by down‑regulating the pituitary LHRH signal.
Because the pathways are different, a patient who stops responding to one class can sometimes be rescued with another.
Side‑Effect Profiles - What to Expect
Side effects often dictate which drug a patient can tolerate long‑term.
- Arimidex, Letrozole, Exemestane: Joint and muscle pain (arthralgia), hot flashes, mild bone loss, and occasional fatigue.
- Tamoxifen: Increased risk of blood clots, endometrial changes, hot flashes, and vaginal discharge.
- Fulvestrant: Injection‑site pain, nausea, and occasional liver‑function abnormalities.
- Goserelin: Menopausal symptoms (hot flashes, mood swings), decreased libido, and occasional injection‑site reactions.
Bone health is a big deal with aromatase inhibitors; many oncologists add calcium, vitaminD, and sometimes bisphosphonates to the regimen.
Comparison Table
| Drug | Class | Typical Dose | FDA Approval Year | Primary Advantage | Common Side Effects |
|---|---|---|---|---|---|
| Arimidex | Aromatase inhibitor (non‑steroidal) | 1mg PO daily | 1995 | Convenient oral dosing, strong estrogen suppression | Arthralgia, hot flashes, bone loss |
| Letrozole | Aromatase inhibitor (non‑steroidal) | 2.5mg PO daily | 1997 | Very high estrogen reduction, useful in neoadjuvant setting | Joint pain, fatigue, hot flashes |
| Exemestane | Aromatase inhibitor (steroidal) | 25mg PO daily | 1999 | Irreversible binding may delay resistance | Muscle aches, nausea, bone loss |
| Tamoxifen | Selective estrogen receptor modulator (SERM) | 20mg PO daily | 1977 | Effective for pre‑menopausal patients, bone‑preserving | Clot risk, endometrial thickening, hot flashes |
| Fulvestrant | Estrogen receptor antagonist | 500mg IM injection | 2002 | Useful after aromatase inhibitor failure | Injection site pain, nausea, liver enzyme rise |
| Goserelin | LHRH agonist | 3.6mg SC every 28days | 1990 | Suppresses ovarian estrogen production, works in pre‑menopausal women | Menopausal symptoms, injection site irritation |
Choosing the Right Option - Practical Decision Guide
Here’s how you can narrow it down based on common scenarios:
- Post‑menopausal, early‑stage cancer: Arimidex, Letrozole, or Exemestane are first‑line. If you have a history of severe joint pain, letrozole’s higher potency might worsen it, so many opt for anastrozole.
- You’re dealing with osteoporosis or low bone density: Tamoxifen actually helps bone, while aromatase inhibitors can accelerate loss. Discuss adding a bisphosphonate or switching to tamoxifen if bone health is a priority.
- Pre‑menopausal and still having menstrual cycles: Aromatase inhibitors won’t work because the ovaries keep pumping estrogen. Options are Tamoxifen, Goserelin (to shut down the ovaries), or a combination.
- Cancer progressed despite an aromatase inhibitor: Switching to a different class-like Fulvestrant or adding Exemestane-can restore control.
- Concern about blood clots: Avoid Tamoxifen if you have clot risk factors; stick with an aromatase inhibitor and monitor bone health.
Always involve your oncologist in the final call; they’ll weigh lab results, imaging, and personal health history.
Monitoring and Adherence Tips
Even the best drug won’t help if you miss doses. Below are a few tricks that patients swear by:
- Set a daily alarm on your phone; the pill is taken at the same time each day.
- Keep a simple log-paper or a note‑taking app-marking each dose.
- Schedule regular bone‑density scans (DEXA) every 1‑2 years if you’re on an aromatase inhibitor.
- Ask your doctor about blood tests for liver function and cholesterol every 3‑6 months.
- If you experience joint pain, try low‑impact exercise (swimming, walking) and discuss NSAIDs or a short course of steroids with your physician.
Frequently Asked Questions
Can I switch from Arimidex to Letrozole without a wash‑out period?
Yes. Because both are non‑steroidal aromatase inhibitors, doctors usually transition directly. Your oncologist will monitor estrogen levels for a few weeks to confirm suppression.
Is Exemestane better for patients with joint pain?
Exemestane’s steroidal structure can be gentler on joints for some people, but results vary. If you’ve struggled with arthralgia on anastrozole or letrozole, a trial of exemestane is worth discussing.
Do aromatase inhibitors increase the risk of heart disease?
Studies show a modest uptick in cholesterol levels, which can translate to higher cardiovascular risk over time. Regular lipid panels and a heart‑healthy diet are recommended.
Why would a doctor prescribe Tamoxifen instead of an aromatase inhibitor?
Tamoxifen works in pre‑menopausal women and also protects bone density. It’s also the go‑to drug for women who can’t tolerate the joint pain or bone loss associated with aromatase inhibitors.
How long do I stay on Arimidex after surgery?
Standard adjuvant therapy lasts five years, either as a single agent or after a short course of tamoxifen. Some trials suggest extending to ten years for high‑risk patients, but that decision is individualized.
In the end, the “best” drug is the one that fits your biology, lifestyle, and treatment goals. Talk openly with your care team, keep track of how you feel, and don’t hesitate to ask for a switch if side effects become unbearable.

Dominique Lemieux
October 4, 2025 AT 13:51When one surveys the aromatic tapestry of estrogen‑directed therapeutics, it becomes evident that the prevailing narrative often glorifies the most market‑driven agents while obscuring the nuanced choreography of molecular interaction. Arimidex, a non‑steroidal aromatase inhibitor, indeed arrests the conversion of androgens to estrogen with a precision that is reminiscent of a seasoned violinist coaxing a perfect note from a restless string. Yet, let us not be blinded by its convenient once‑daily dosing; the very potency that suppresses estrogen by 97 % also ushers in a cascade of physiological reverberations that echo through bone, joints, and even the psyche. Letrozole, though sharing a structural kinship, wields a slightly higher affinity for the aromatase pocket, a fact that may translate into a marginally deeper estrogen nadir, but also a propensity for more vivid hot flashes. Exemestane, the steroidal outlier, binds irreversibly, a molecular suicide pact that can circumvent the adaptive resistance observed with its non‑steroidal cousins, yet it carries its own specter of musculoskeletal discomfort. Tamoxifen, the venerable SERM, offers a paradoxical duality: antagonism within the breast juxtaposed with agonistic whispers in bone and the uterus, a dance that can be both protective and perilous depending on the patient’s clotting proclivities. Fulvestrant, delivered by the blunt instrument of intramuscular injection, demolishes estrogen receptors altogether, providing a salvage pathway for those whose disease has outwitted oral agents. Goserelin, by silencing the hypothalamic‑pituitary‑ovarian axis, redefines the menopausal state for pre‑menopausal women, yet the abrupt hormonal vacuum can precipitate a cascade of vasomotor and mood disturbances. The clinician’s challenge, therefore, is not merely to select a drug from a spreadsheet, but to orchestrate a symphony of patient‑specific variables-bone mineral density, cardiovascular risk, prior joint pain, and personal preferences-into a harmonious regimen that sustains both survival and quality of life. One must weigh the specter of osteoporosis against the convenience of an oral pill, the allure of a once‑monthly injection against the dread of injection‑site pain, and the specter of clotting against the comfort of bone preservation. In the end, the “best” drug is a personalized equilibrium, a compromise struck not in a vacuum but within the lived reality of each individual patient.
Laura MacEachern
October 5, 2025 AT 17:38Great overview! If you’re juggling bone health concerns, remember that calcium and vitamin D supplementation can really help offset the bone loss some aromatase inhibitors cause.
BJ Anderson
October 6, 2025 AT 21:24The hormonal landscape is a battlefield where each drug brings its own artillery. Arimidex’s steady daily strike is reliable, yet some patients feel its joint aches like tiny artillery shells muttering under their skin. Letrozole cranks up the estrogen blockade, sometimes at the cost of amplified hot flashes. Exemestane’s irreversible binding can feel like a one‑time treaty-effective but not without its own side‑effects chorus. Ultimately, the choice hinges on how your body’s unique ecosystem reacts to each assault.
Alexander Rodriguez
October 8, 2025 AT 01:11Arimidex, Letrozole, and Exemestane all hit the same target, but they differ in dosage and side‑effect profiles. If you’ve got joint pain, you might prefer Exemestane’s steroidal nature. Otherwise, the non‑steroidal agents are usually first‑line.
Abhinav Sharma
October 9, 2025 AT 04:58The decision matrix can feel like a labyrinth, but think of it as a guided tour 😊. Bone‑preserving options like Tamoxifen shine when osteoporosis looms, while aromatase inhibitors excel in post‑menopausal settings. Adding a bisphosphonate can be a wise side‑quest for those on Arimidex or Letrozole. Keep an eye on lipid panels, as aromatase inhibition may nudge cholesterol upward.
Welcher Saltsman
October 10, 2025 AT 08:44just a heads up that staying consistent with the daily pill is key, missing doses can throw off estrogen suppression and mess with outcomes. set an alarm or pair it with a daily habit like brushing teeth. also, regular DEXA scans help catch bone loss early.
april wang
October 11, 2025 AT 12:31When navigating the sea of endocrine therapies, it is vital to chart a course that respects both the clinical evidence and the individual’s lived experience. Arimidex offers the simplicity of a single daily tablet, which can be a boon for adherence, yet its propensity for arthralgia should not be dismissed as a mere inconvenience. Letrozole’s heightened estrogen suppression may provide marginal efficacy gains in certain high‑risk cohorts, but the trade‑off often manifests as intensified joint discomfort and fatigue. For patients whose skeletal health is already compromised, Tamoxifen’s partial agonist activity in bone can act as a protective anchor, albeit at the expense of an increased clotting risk that must be vigilantly monitored. Exemestane’s irreversible binding presents an intriguing option for those who have encountered resistance to non‑steroidal agents, though clinicians should balance this against its own gastrointestinal and musculoskeletal side‑effects. In the realm of advanced disease, Fulvestrant’s mechanism of receptor degradation can rescue patients whose tumors have outmaneuvered aromatase inhibition, but the requirement for intramuscular administration may affect quality‑of‑life considerations. Goserelin, by suppressing ovarian estrogen output, remains the cornerstone for pre‑menopausal patients, yet the induced menopausal symptoms demand comprehensive supportive care. Ultimately, the optimal therapeutic strategy is an evolving tapestry woven from tumor biology, comorbid conditions, patient preferences, and the vigilant stewardship of side‑effect mitigation strategies.
Vishnu Raghunath
October 12, 2025 AT 16:18Oh sure, just pop a pill and the cancer disappears-if only reality were that simple. The pharma machine loves the myth.
Aparna Dheep
October 13, 2025 AT 20:04One must recognize that the discourse surrounding hormonal agents is often reduced to a binary of efficacy versus toxicity, neglecting the profound philosophical implications of mediating a woman’s identity through pharmaceutical means. The commodification of such intimate processes, while cloaked in scientific rigor, subtly enforces a cultural hegemony that privileges certain narratives of survivorship over others.
Nicole Powell
October 14, 2025 AT 23:51Choosing a drug based on side‑effect profiles is the only rational approach.
Ananthu Selvan
October 16, 2025 AT 03:38Honestly this whole debate is a waste of energy-pick a drug and move on.
Nicole Chabot
October 17, 2025 AT 07:24It's encouraging to see such a thorough breakdown, and it really helps demystify the options for anyone starting this journey.
Vivek Koul
October 18, 2025 AT 11:11Building on the earlier discussion of bone health, it is worth emphasizing that regular monitoring of bone mineral density, coupled with proactive supplementation and, when indicated, the judicious use of bisphosphonates or denosumab, can markedly reduce the risk of fractures associated with aromatase inhibitor therapy. Such a comprehensive approach aligns clinical efficacy with the preservation of overall well‑being.