Antihistamines and Blood Pressure: Effects, Risks, and Monitoring Guide
 Oct, 25 2025
Oct, 25 2025
Antihistamine Blood Pressure Impact Calculator
How Antihistamines Affect Your Blood Pressure
Select your antihistamine type to see potential blood pressure effects and recommended monitoring schedule.
Results
Ever wondered whether your daily allergy pill could nudge your blood pressure up or down? Below you’ll get a straight‑forward rundown of how antihistamines interact with blood pressure, which drugs are safest for a hypertensive patient, and what simple monitoring steps keep you on the safe side.
Key Takeaways
- Pure H1‑blocking antihistamines have antihistamines blood pressure impact that is usually neutral.
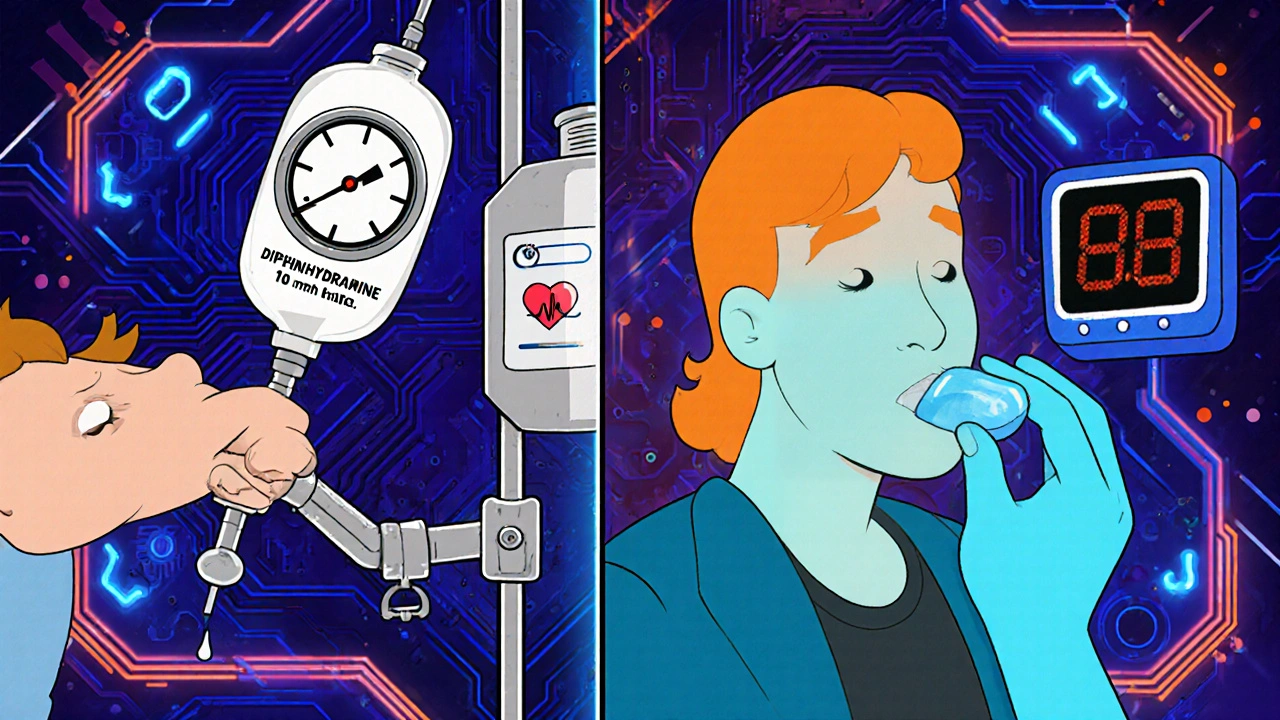
- First‑generation agents (e.g., diphenhydramine) can cause mild hypotension when given intravenously and may trigger a brief tachycardia.
- Second‑generation drugs (loratadine, cetirizine, fexofenadine) are considered cardiovascular‑safe for most hypertensive patients.
- Combination products that add pseudo‑ephedrine, ibuprofen or acetaminophen can raise systolic pressure by 1‑5 mmHg.
- Baseline BP check, a follow‑up reading 30‑60 minutes after the first dose (first‑gen only), and symptom‑driven monitoring thereafter are recommended.
Antihistamines are pharmacologic agents that block histamine receptors, primarily H1 and H2, to alleviate allergic symptoms such as itching, swelling, and runny nose. They fall into two major classes - first‑generation and second‑generation - each with distinct pharmacokinetic traits that shape their cardiovascular profile.
How Histamine Influences Blood Vessels
When an allergen triggers mast cells, Histamine floods the local tissue. By binding to H1 receptor, it causes vasodilation, increased vascular permeability, and smooth‑muscle contraction. This cascade can lower systemic vascular resistance for a short spell, which is why an acute allergic reaction sometimes feels like a “drop” in blood pressure.
First‑Generation vs. Second‑Generation Antihistamines
The classic first‑generation drugs (diphenhydramine, chlorpheniramine) cross the blood‑brain barrier, have a short half‑life (4-6 hours), and are metabolised by CYP2D6 and CYP3A4. Their anticholinergic activity can produce transient tachycardia, dry mouth, and, when given intravenously, an 8‑12 mmHg systolic dip within 15 minutes.
Second‑generation agents (loratadine, cetirizine, fexofenadine) stay mostly peripheral, last 12-24 hours, and rely mainly on CYP3A4. Clinical trials up to 2022 show neutral effects on systolic and diastolic numbers in >95 % of hypertensive volunteers.
| Property | First‑Generation | Second‑Generation |
|---|---|---|
| Typical BP change (oral) | 0 ± 2 mmHg (neutral) but occasional tachycardia | 0 ± 1 mmHg (neutral) |
| IV‑induced hypotension | ‑8 to ‑12 mmHg systolic within 15 min | Not applicable (IV forms rare) |
| Metabolism pathway | CYP2D6, CYP3A4 | CYP3A4 (minimal CYP2D6) |
| Blood‑brain barrier penetration | High | Low |
| Common adverse cardiac effect | Transient tachycardia, rare hypotension | None reported in large trials |
Spotlight on Popular Agents
Diphenhydramine (Benadryl) is the go‑to first‑gen drug for night‑time allergy relief. Its anticholinergic load can make patients feel drowsy, and IV bolus in allergy testing has been linked to measurable drops in blood pressure that resolve after observation.
Loratadine (Claritin) tops the second‑generation list. A 2022 FDA‑review of 97 % of trials found no statistically significant BP shift, even in patients on multiple antihypertensives.
Fexofenadine (Allegra) is a metabolite of the withdrawn terfenadine. Because it bypasses CYP3A4, drug‑drug interaction risk is low, and cardiovascular safety mirrors loratadine.
When Combination Products Raise the Stakes
Many over‑the‑counter cold formulas mix an H1 blocker with a decongestant such as pseudo‑ephedrine. The latter raises systolic pressure by about 1 mmHg on its own, but in hypertensive patients the rise can reach 5‑10 mmHg, especially if the dose hits the upper OTC limit.
Acetaminophen, ibuprofen, or other analgesics added for pain can also lift BP modestly (up to 5 mmHg with high‑dose ibuprofen). For a patient already walking the fine line of control, these increments matter.
Monitoring Protocols You Can Use at Home or Clinic
The American Heart Association (2022) suggests a simple three‑step routine:
- Take a baseline reading before the first antihistamine dose.
- For first‑generation oral tablets, re‑measure 30‑60 minutes after the dose; for IV administration, wait 15 minutes.
- If the patient reports dizziness, headache, or palpitations, record a second reading 2‑4 hours later and contact a clinician.
Second‑generation users generally need only a follow‑up if they have known cardiovascular disease, are on multiple antihypertensives, or notice unusual symptoms.
Validated home monitors (cuff‑style, automatic) are preferred. Record three consecutive readings each time and keep a log for at least three days before and after starting the medication.
Special Situations to Watch
- Renal or hepatic impairment: Reduced clearance can raise plasma levels, especially for diphenhydramine. Dose‑adjust or switch to a second‑gen agent.
- Concomitant CYP3A4 inhibitors: Drugs like ketoconazole or erythromycin can elevate loratadine or fexofenadine levels, potentially altering vascular tone.
- Genetic polymorphisms: About 14 % of the population carry CYP2D6 variants that slow diphenhydramine metabolism, making hypotension more likely.
- Pregnancy: Second‑gen agents are category B in the US; first‑gen should be avoided unless benefits outweigh risks.
Practical Tips for Patients and Clinicians
- Ask your pharmacist whether the product contains a decongestant.
- Prefer once‑daily second‑generation antihistamines for chronic control.
- Keep a symptom diary for the first week - note any light‑headedness, chest discomfort, or new headaches.
- If you use an IV dose for allergy testing, stay in the clinic for at least 30 minutes for observation.
- When switching from a first‑gen to a second‑gen drug, no washout period is needed, but re‑check BP 24 hours after the change.
Future Directions
Research now eyes selective H3 agonists as possible cardioprotective agents, and pharmacogenomic panels are being rolled out in several health systems to flag at‑risk CYP2D6 or CYP3A4 carriers before prescribing antihistamines.
Bottom Line
For most people with hypertension, a plain second‑generation antihistamine is as safe as a glass of water. Problems usually arise when the drug is mixed with a decongestant, when it’s given intravenously, or when the patient has liver/kidney disease or takes strong CYP inhibitors. A quick baseline BP check and a follow‑up reading after the first dose give you peace of mind without a lot of hassle.
Can antihistamines raise my blood pressure?
Pure H1‑blocking antihistamines (like loratadine or cetirizine) generally have a neutral effect on blood pressure. Only combination products that contain pseudo‑ephedrine or NSAIDs tend to raise systolic pressure by a few millimetres.
Should I monitor my blood pressure after taking diphenhydramine?
Yes. Take a baseline reading, then check again 30‑60 minutes after the oral dose. If you receive it intravenously, re‑measure at 15 minutes and observe for 30 minutes.
Is it safe to use a cold medicine that contains pseudo‑ephedrine if I have hypertension?
Use caution. Pseudo‑ephedrine can add 1‑5 mmHg to systolic pressure, which may push borderline patients into uncontrolled ranges. Talk to your doctor before using such products.
Do I need a doctor’s order to get an over‑the‑counter antihistamine?
No prescription is required for most second‑generation antihistamines. However, if you have severe hypertension, heart disease, or are on multiple medications, a clinician’s guidance is advisable.
What should I do if I feel dizzy after taking an antihistamine?
Stop the medication, sit or lie down, and re‑measure your blood pressure. If the reading is low (<90 mmHg systolic) or symptoms persist, seek medical attention.

Kevin Stratton
October 26, 2025 AT 18:33Imagine the body as a finely tuned orchestra, each instrument playing its part while the conductor-your nervous system-keeps the tempo steady 🙂. When you pop a second‑generation antihistamine, it steps in like a quiet violin, silencing the allergic crescendo without demanding the brass section to shift its pitch. The result is a neutral blood‑pressure reading, a subtle harmony that most hypertensive patients can trust. Of course, the occasional first‑gen cameo may introduce a fleeting tachycardic solo, but the overall symphony remains balanced.
Manish Verma
October 26, 2025 AT 19:23Look, mates, if you think you can ignore the decongestant sneaking into your cold medicine, you’re just handing over control to corporate profit‑driven chemists. Those pseudo‑ephedrine add‑ons are like rogue drummers beating a louder rhythm on a calm track, pushing systolic numbers up for anyone with a borderline BP. It’s not just “a little rise” – it’s a deliberate gamble that many folks in our country can’t afford. So ditch the combo pills and stick to the pure H1 blockers; your heart will thank you.
Lionel du Plessis
October 26, 2025 AT 21:20first‑gen antihistamines cross BBB high metabolism CYP2D6 CYP3A4 leads to transient tachycardia low‑dose iv drop 8‑12mmhg second‑gen stay peripheral neutral effect on systolic/diastolic especially in hypertensive cohort
Andrae Powel
October 26, 2025 AT 22:26That’s a solid rundown of the pharmacokinetics. For anyone juggling hypertension meds, the safest move is to start with a once‑daily loratadine or cetirizine, record a baseline BP, then check again after the first dose. If you notice any dizziness, log that reading and give your clinician a heads‑up. This simple routine keeps you in control without extra appointments.
Leanne Henderson
October 27, 2025 AT 00:06Hey there, just wanted to say, you’re doing great, keep listening to your body, and remember, a quick baseline reading before you start any new antihistamine is a tiny step that can make a huge difference, especially if you have a history of high blood pressure, and if you ever feel a little light‑headed, don’t panic – just sit down, re‑measure, and reach out to your doctor if it doesn’t improve, okay?
Megan Dicochea
October 27, 2025 AT 00:15Just watch your numbers.
Edward Brown
October 27, 2025 AT 01:30Ever wonder why the pharma giants push combo cold meds so hard? they want you to rely on over‑the‑counter fixes while they collect data on your vitals, subtle shifts in blood pressure feed into larger studies, and the more you use, the more they can market “new” formulations, all while the real risk stays hidden behind flashy ads and vague warnings, keep your eyes open.
Kala Rani
October 27, 2025 AT 02:03Sure, but the data actually shows most users never see a dangerous spike, so maybe the hype is overblown.
eko lennon
October 27, 2025 AT 02:53In the grand theatre of daily life, where the curtain rises on the mundane chorus of sneezes, tears, and the occasional sniffle, there emerges a protagonist unlike any other-a humble antihistamine, poised on the edge of the stage, beckoning us to consider the silent drama unfolding within our very veins. As the spotlight shifts to the first‑generation cast, we witness a fleeting yet palpable dip in systolic pressure, a momentary bow that whispers of ancient mechanisms, a reminder that even the most familiar drugs can wield a subtle, almost theatrical influence on cardiovascular rhythm. Yet, in stark contrast, the second‑generation ensemble steps onto the scene with a confidence that borders on the regal, delivering a performance so steady and composed that the audience-a collective of hypertensive patients-finds solace in its predictable cadence. The narrative does not end with mere pharmacology; it stretches into the realm of patient empowerment, urging each individual to become the director of their own health saga, clutching a home‑monitoring cuff like a script, ready to annotate every beat and every subtle rise. It is here, in those three simple steps-baseline, post‑dose, symptom‑triggered follow‑up-that the plot thickens, transforming a routine medication routine into a meticulous, almost cinematic, chronicle of self‑care. When the curtain falls on the discussion of pseudo‑ephedrine‑laden concoctions, the audience is left to contemplate the weight of each millimetre of mercury, an invisible yet potent antagonist that can tip the scales from control to chaos. The irony, dear readers, lies in the fact that a mere over‑the‑counter tablet can masquerade as a harmless ally while subtly rewriting the script of blood pressure regulation. Thus, the wise clinician, akin to a seasoned playwright, must guide the protagonist-be it loratadine, cetirizine, or fexofenadine-through the labyrinth of comorbidities, renal concerns, and pharmacogenomic nuances, ensuring that no rogue line derails the harmony of the piece. In a world where health narratives are often penned in rushed footnotes, this guide stands as a testament to the power of deliberate, measured storytelling, inviting each of us to become the hero of our own physiological drama, armed with knowledge, vigilance, and a steadfast commitment to balance. And so, as the final applause fades, we are left with a lingering question, not of doubt, but of resolve: will you, dear reader, step onto the stage, cuff in hand, ready to conduct the symphony of your blood pressure with the poise of a maestro?
Sunita Basnet
October 27, 2025 AT 04:16Keep it simple stay proactive! Use an validated cuff log your three readings daily and watch trends, no need for fancy labs unless you notice a spike, remember second‑gen antihistamines are cardio‑safe, and if you ever add a decongestant, just double‑check your numbers, you’ve got this!