Amiloride Drug Interactions: Complete Review & Management Guide
 Oct, 15 2025
Oct, 15 2025
Amiloride Hyperkalemia Risk Calculator
Assess Your Hyperkalemia Risk
Enter key factors to evaluate your risk of hyperkalemia while taking amiloride.
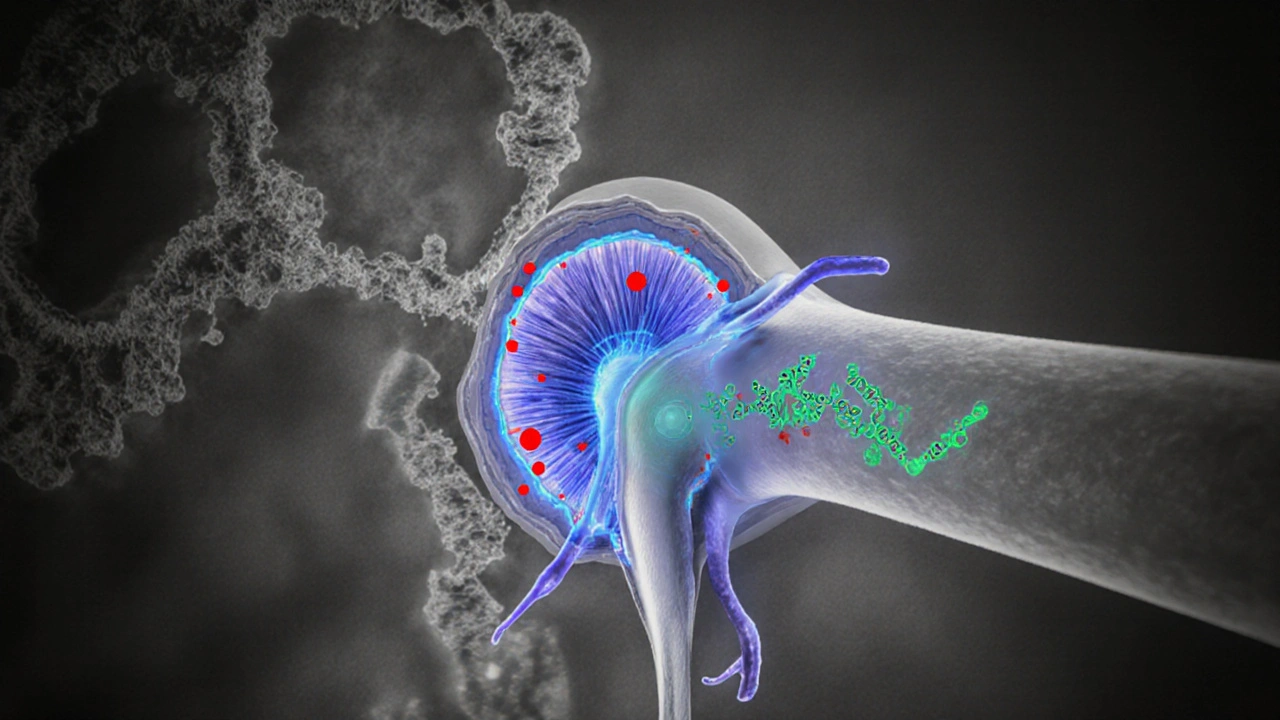
When taking amiloride, it’s crucial to understand how this medication works. Amiloride is a potassium‑sparing diuretic that blocks epithelial sodium channels (ENaC) in the distal nephron, reducing sodium reabsorption while conserving potassium. This balance makes it a handy tool for hypertension, heart failure, and certain cases of edema, but it also opens the door to a host of drug interactions.
How Amiloride Works in the Body
Amiloride targets the ENaC located in the late distal convoluted tubule and collecting duct. By inhibiting these channels, it ↓ sodium uptake and ↑ water excretion, yet potassium remains largely unchanged because the drug spares its loss. Oral bioavailability sits around 50%, peak plasma levels appear in 1-2hours, and the drug is eliminated unchanged via the kidneys.
Primary Clinical Uses
- Adjunct therapy for resistant hypertension.
- Management of volume overload in heart failure when other diuretics cause hypokalemia.
- Prevention of potassium loss in patients on thiazide or loop diuretics.
Key Drug Interaction Categories
Because amiloride touches the kidney’s fine‑tuned electrolyte system, several drug classes can tip the balance toward danger.
1. ACE Inhibitors and ARBs
ACE inhibitor drugs that block the conversion of angiotensin I to angiotensin II, promoting vasodilation and potassium retention already raise serum potassium. Adding amiloride can push levels into the hyper‑kalemic range, especially in patients with renal impairment.
2. Non‑steroidal Anti‑Inflammatory Drugs (NSAIDs)
NSAID inhibits prostaglandin synthesis, reducing renal blood flow and impairing potassium excretion. The combo may blunt the diuretic effect of amiloride and heighten the risk of acute kidney injury.
3. Lithium
Lithium a mood stabilizer cleared primarily by the kidneys; its reabsorption rises when sodium transport is blocked. Amiloride can raise lithium concentrations up to 2‑fold, leading to tremor, nausea, or even lithium toxicity.
4. Cyclosporine
Cyclosporine an immunosuppressant that also reduces renal potassium excretion. When paired with amiloride, clinicians often see synergistic hyperkalemia.
5. Digoxin
Digoxin a cardiac glycoside whose toxicity is potentiated by high serum potassium. While low potassium predisposes to digoxin‑induced arrhythmias, excessive potassium from amiloride can blunt its therapeutic effect and obscure toxicity signs.
6. Other Diuretics
Combining amiloride with thiazides or loop diuretics is common to counteract potassium loss, but dose‑timing matters. Over‑suppression of sodium reabsorption can precipitate severe hyponatremia or volume depletion.
Clinical Consequences of Major Interactions
- Hyperkalemia: Serum potassium >5.5mmol/L can cause muscle weakness, cardiac arrhythmias, and, in extreme cases, cardiac arrest.
- Renal Impairment: NSAIDs or ACE inhibitors combined with amiloride may cause a rise in serum creatinine >30%.
- Lithium Toxicity: Levels >1.2mmol/L often present with tremor, ataxia, and confusion.
- Reduced Diuretic Efficacy: NSAIDs may blunt natriuresis, leading to persistent edema.
Managing Interactions: Practical Strategies
- Baseline labs: Check serum potassium, creatinine, and eGFR before starting amiloride.
- Medication review: Identify ACE inhibitors, ARBs, NSAIDs, lithium, cyclosporine, digoxin, and other diuretics in the patient’s list.
- Dose adjustment: If an ACE inhibitor is required, consider starting amiloride at 2.5mg daily and increase only after confirming potassium <5.0mmol/L.
- Monitoring schedule: Re‑check potassium and renal function 1week after initiation, then monthly for the first 3months.
- Patient counseling: Advise on signs of hyperkalemia (muscle tingling, irregular heartbeat) and the importance of staying hydrated.
- Alternative choices: For patients on lithium, consider switching the diuretic to a thiazide with close lithium level monitoring.

Quick Interaction Reference Table
| Interacting Drug/Class | Effect on Potassium | Renal Impact | Management Tip |
|---|---|---|---|
| ACE inhibitor / ARB | ↑↑ | Potential rise in creatinine | Start low‑dose amiloride; monitor K⁺ & creatinine |
| NSAID | Variable (can ↑ K⁺) | Decreased renal perfusion | Avoid chronic NSAID use; consider COX‑2 selective if needed |
| Lithium | ↑↑ (Lithium levels rise) | Risk of nephrotoxicity | Reduce lithium dose by 25% or switch diuretic |
| Cyclosporine | ↑↑ | Nephrotoxic synergy | Frequent K⁺ checks; consider alternative immunosuppressant |
| Digoxin | ↑ (may mask toxicity) | None direct | Check digoxin level if K⁺ >5.5mmol/L |
| Thiazide / Loop diuretic | Counteracts K⁺ loss | Enhanced natriuresis | Stagger dosing; avoid simultaneous high‑dose use |
Prescriber Checklist
- Confirm indication for amiloride.
- Document all concurrent medications (especially ACEI/ARB, NSAID, lithium).
- Order baseline labs: K⁺, Na⁺, creatinine, eGFR.
- Choose initial dose (2.5mg once daily for most adults).
- Set follow‑up lab schedule: 1week, 1month, then quarterly.
- Educate patient on diet (avoid high‑potassium foods if risk).
- Adjust dose or discontinue amiloride if K⁺ >5.5mmol/L or creatinine rises >30%.
Frequently Asked Questions
Can I take over‑the‑counter NSAIDs with amiloride?
Occasional short‑term NSAID use (e.g., ibuprofen for a few days) is usually safe if you have normal kidney function and your potassium is within range. Chronic NSAID therapy, however, increases the risk of hyperkalemia and renal impairment, so it should be avoided or closely monitored.
Why does amiloride raise lithium levels?
Amiloride blocks sodium reabsorption in the distal tubule, which also reduces lithium’s excretion. Less lithium is cleared, so blood levels climb, often requiring a dose reduction of 25‑30% or switching to a different diuretic.
What potassium level is considered dangerous while on amiloride?
A serum potassium above 5.5mmol/L is generally flagged as hyperkalemia. Symptoms may include muscle weakness, tingling, or irregular heartbeat. If it exceeds 6.0mmol/L, urgent medical attention is needed.
Do I need to stop amiloride before surgery?
Most surgeons recommend holding amiloride 24‑48hours before major surgery, especially if anesthesia or fluid shifts could affect kidney function. Always follow your peri‑operative team’s advice.
Is amiloride safe for people with chronic kidney disease (CKD)?
In early CKD (stage1‑2) it can be used cautiously with frequent lab monitoring. In advanced CKD (stage4‑5) the risk of hyperkalemia rises sharply, and many clinicians avoid it altogether.

RONEY AHAMED
October 15, 2025 AT 19:22Just a heads‑up: before you start amiloride, grab a baseline BMP and keep an eye on that potassium. Even a modest rise can sneak up if you’re also on an ACE inhibitor.
emma but call me ulfi
October 16, 2025 AT 09:33I like how the guide lays out the checklist – having a clear step‑by‑step lab schedule can really lower anxiety for patients who are new to diuretics.
George Gritzalas
October 16, 2025 AT 23:26Wow, someone actually wrote "potassium" with a capital "K" in the middle of a sentence – guess we’re all about that peak‑shouting style now.
Jeremy Laporte
October 16, 2025 AT 23:43Hey, no need to get all caps‑crazy. The important thing is to remember that labs are the safety net, not a suggestion. Keep it casual, keep it consistent.
Glenn Gould
October 17, 2025 AT 13:20Stay chill, check K+.
Julien Martin
October 18, 2025 AT 17:06From a pharmacokinetic standpoint, amiloride’s 50% oral bioavailability means that half the dose actually reaches the distal nephron where it exerts its ENaC‑blocking effect. Because the drug is eliminated unchanged by the kidneys, renal function directly modulates systemic exposure; a reduced eGFR can effectively double plasma concentrations. This is why the interaction with ACE inhibitors and ARBs is not merely additive but synergistic – both drug classes independently curb sodium reabsorption while sparing potassium, pushing serum K+ toward the hyperkalemic range. When NSAIDs enter the mix, prostaglandin synthesis inhibition reduces renal perfusion, which can blunt the natriuretic response of amiloride and simultaneously impair potassium excretion. The lithium‑amiloride story is a classic example of tubular reabsorption competition: blocking sodium uptake in the collecting duct also traps lithium, raising its plasma level potentially two‑fold. Clinicians should therefore pre‑emptively lower lithium dosage by roughly 25 % when initiating amiloride. Cyclosporine’s nephrotoxic profile adds another layer; its effect on renal vasoconstriction compounds the risk of hyperkalemia, especially in patients with baseline CKD. Digoxin toxicity dynamics flip depending on serum potassium – low K+ predisposes to arrhythmogenic digoxin effects, while high K+ can mask toxicity signs, making monitoring even more critical. Combining amiloride with thiazides or loops is routine to balance potassium, but timing matters: staggering doses by several hours can prevent an abrupt plunge in sodium that would otherwise trigger orthostatic hypotension. In practice, a baseline BMP, followed by repeat labs at one week and one month, captures most clinically relevant shifts. Patient education should also emphasize dietary potassium control – foods like bananas, avocados, and tomatoes can tip the balance in susceptible individuals. Finally, peri‑operative management often calls for holding amiloride 24–48 hours prior to major surgery to avoid intra‑operative electrolyte swings.
Lolita Rosa
October 18, 2025 AT 17:40Honestly, reading that deep dive makes me proud that American clinicians keep pushing the science forward, even if the paperwork feels endless. It’s a testament to our commitment to patient safety.
Sudha Srinivasan
October 19, 2025 AT 20:53One must always prioritize caution; reckless prescribing leads to avoidable suffering.
Jesse Stubbs
October 19, 2025 AT 21:10Ugh, another endless checklist. People love to act like they’re writing a novel when a simple dose adjustment would do.